Emergency Medicine: All Areas
Emergency Medicine 14
372 - A review of patient population utilizing novel critical care pediatric transport stroke clinical practice guideline: a three-year single site analysis
Publication Number: 372.405
.jpg)
Elizabeth W. Perry, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
University of Texas Southwestern/Children's Medical Center
Carrollton, Texas, United States.jpg)
Elizabeth W. Perry, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
University of Texas Southwestern/Children's Medical Center
Carrollton, Texas, United States
Presenting Author(s)
First Author(s)
Background:
Pediatric acute ischemic stroke is a rare diagnosis that requires timely recognition and management to prevent morbidity and mortality. The Children’s Mercy Hospital Critical Care Transport Team (CMCCT) created a novel clinical practice guideline (CPG) for suspected acute ischemic stroke. This retrospective study describes patients < 18 years who met criteria for the novel CPG by CMCCT.
Objective:
To describe patients meeting criteria for activation of novel pediatric critical care transport CPG for suspected acute ischemic stroke including demographic data and presenting symptoms. Secondary objective includes calculation of validated adult stroke scoring modalities to determine usefulness of these scores for prediction of acute ischemic stroke in the pediatric population.
Design/Methods:
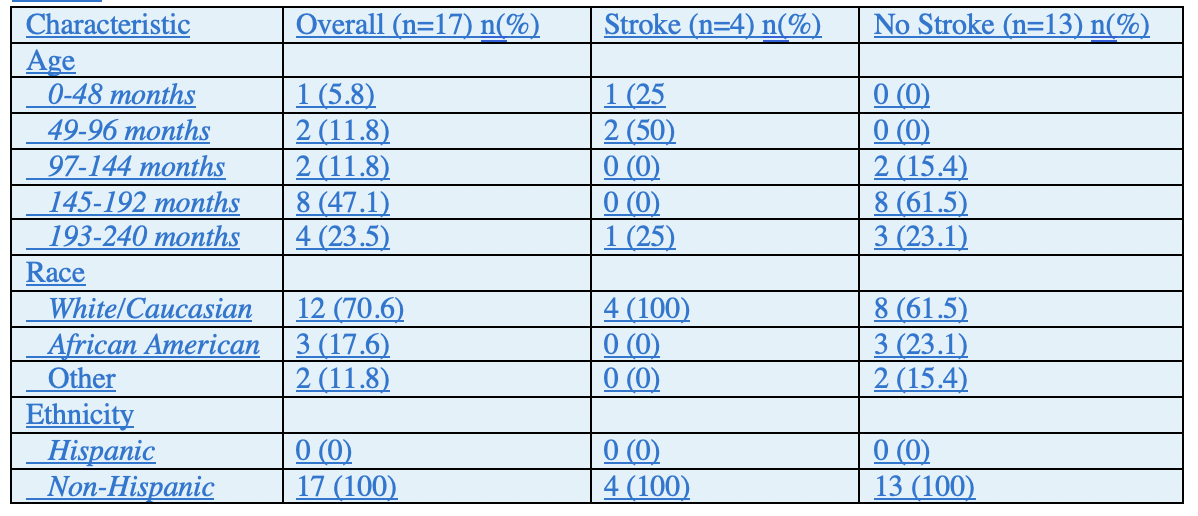
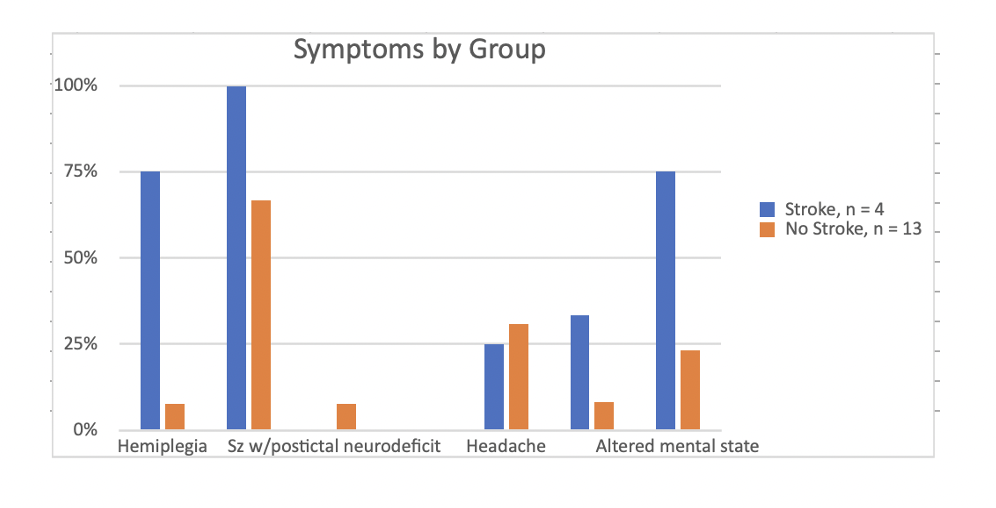
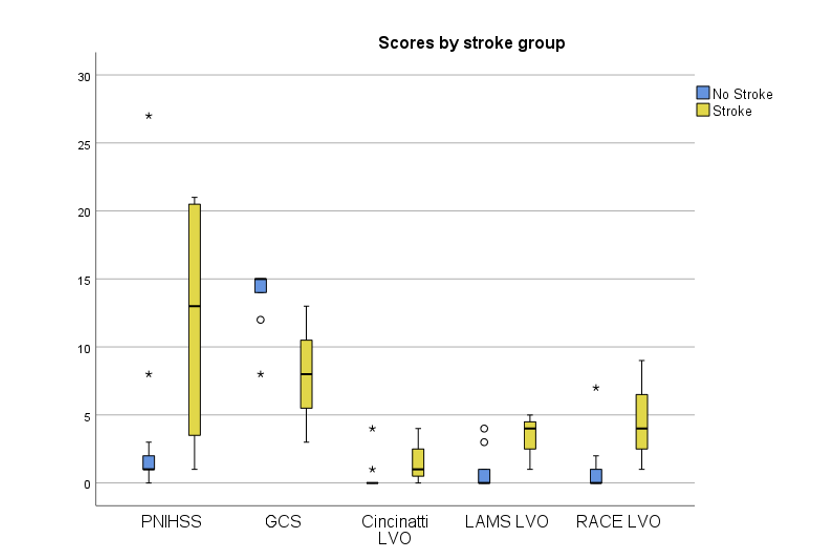
A retrospective chart review was performed of patients transported by CMCCT from September 2016 to March 2020 who met criteria for use of the acute ischemic stroke CPG. Demographic data was extracted from the patient chart. PNIHSS and LVO were retrospectively calculated. Demographics, PNIHSS, LVO scores, and GCS were compared in patients with confirmed acute ischemic stroke to those without confirmed acute ischemic stroke. 17/17,244 (0.001%) pediatric patients transported by CMCCT met criteria for the novel CPG. 4/17 patients (23.5%) had radiographic evidence of thrombus and 3/4 (75%) received alteplase or endovascular clot retrieval. 100% (4/4) of patients with confirmed stroke presented with dysarthria compared to 66.7% (9/13) in the non-stroke group. 75% (3/4) patients with confirmed stroke presented with hemiplegia compared to 7.7% (1/13) of the non-stroke group, p=0.022. 75% (3/4) patients with confirmed stroke presented with altered mental status compared to 23.1% (3/13) patients of the non-stroke group, p=0.099. Headache was seen in 25% (1/4) patients with confirmed stroke compared to 30.8% (4/13) of the non-stroke group, p=1. Seizure was seen in 0/4 (0%) patients with confirmed stroke and 7.7% (1/13) of patients in the non-stroke group, p=1.
Results:
The confirmed stroke group had a lower GCS (median 8 vs. 15, p=0.014), higher LAMS LVO score (median 4 vs. 0, p = 0.021) and higher RACE LVO (median 4 vs. 0, p = 0.036).
Conclusion(s):
Acute ischemic stroke is rare in pediatric patients but remains a time-critical diagnosis. Symptoms described in a clinical practice guideline used by transport systems can lead to recognition of potential stroke that may lead to timely management. Adult validated LVO scoring is not validated in children but can be helpful in triage of pediatric patients.