Neonatal Cardiac Physiology/Pathophysiology/Pulmonary Hypertension
Neonatal Cardiac Physiology/Pathophysiology/ Pulmonary Hypertension 3
94 - Prognostic Value of Echocardiographic Parameters in Congenital Diaphragmatic Hernia: A Systematic Review and Meta-analysis
Publication Number: 94.425

Mohan Pammi, MD, PhD, MRCPCH (he/him/his)
Professor
Baylor College of Medicine
Bellaire, Texas, United States
Presenting Author(s)
Background:
Accurate prognostication of mortality and need for ECMO in infants with Congenital Diaphragmatic Hernia (CDH) can inform clinical management, transfer to an ECMO center and parent counselling.
Objective:
To determine the prognostic value of echocardiographic markers for mortality and need for ECMO in infants with CDH without other major congenital anomalies.
Design/Methods:
We performed the systematic review according to PRISMA guidelines
DATA SOURCES: We searched the electronic databases Ovid-MEDLINE, Embase, Scopus, CINAHL, the Cochrane library and conference proceedings up to July 2022.
STUDY SELECTION: Studies evaluating the prognostic performance of echocardiographic parameters in the diagnosis and management of CDH in term and preterm infants.
DATA EXTRACTION AND SYNTHESIS: Risk of bias and applicability were assessed using QUIPS tool. We used a random effects model for meta-analysis to compute mean differences (MD) for continuous outcomes and relative risk (RR) for binary outcomes with 95% confidence intervals (CI).
MAIN OUTCOMES AND MEASURES: Our primary outcome was mortality and secondary outcomes were need for ECMO, duration of ventilation, length of stay and need for oxygen and/or inhaled nitric oxide.
Results: Twenty-six observational studies were included, and the methodological quality was adequate except for 2 studies. Meta-analysis of the 2-3 studies reporting adequate information, the diameters right pulmonary artery at birth (mm) [MD 0.95 (95% CI 0.45, 1.46)], diameter of left pulmonary artery at birth (mm) [MD 0.79 (0.58, 0.99), left ventricular dysfunction [ RR 2.40 (1.98, 2.91)], right ventricular dysfunction [RR 1.83 (1.29, 2.60)] and severe pulmonary hypertension [RR1.69 (1.53, 1.86)] were useful in prognosticating survival, whereas L/R pulmonary artery ratio [MD -0.03 (-0.19, 0.12)], heart rate (beats per minute) [MD 0.44 (-13.21, 14.10)], systolic duration (seconds) [MD -0.01 (-0.03, 0.01)] and diastolic duration (seconds) [MD -0.00 (-0.07, 0.07)] were not useful. Left ventricular dysfunction [ RR 3.30 (2.19, 4.98)] and right ventricular dysfunction [RR 2.16 (1.85, 2.52)] were useful in prognosticating the need for ECMO.
Conclusion(s):
Left and right ventricular dysfunction, pulmonary hypertension and pulmonary artery diameter are useful prognostic factors among CHD patients. There is a need for consensus on optimal selection and timing of echocardiographic parameters for prognostication, which should be evaluated in large, well-designed trials. 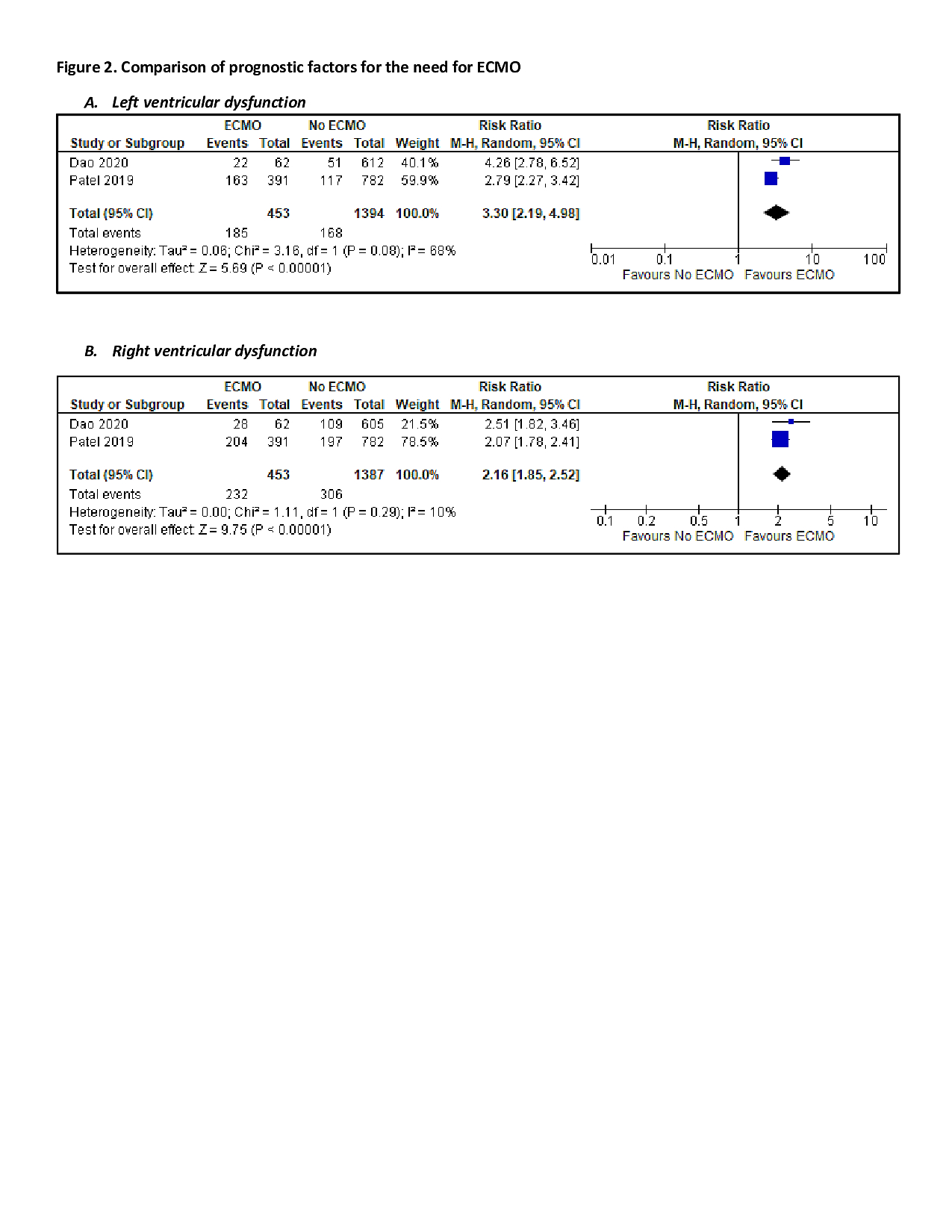
.jpg)
