Medical Education: Resident
Medical Education 13: Resident 4
472 - A Quality Improvement Curriculum with Experiential Learning and Coaching for Pediatric Residents
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 472
Publication Number: 472.421
Publication Number: 472.421
Brandy M. Hoyt, Children's Hospital Colorado, Aurora, CO, United States; Maya Balakrishnan, University of South Florida, Tampa, FL, United States; Fauzia Shakeel, Johns Hopkins All Children's Hospital, St. Petersburg, FL, United States; Kimberly O'Hara, Children's Hospital Colorado, Denver, CO, United States

Brandy M. Hoyt, MD (she/her/hers)
PHM Fellow
Children's Hospital Colorado
Aurora, Colorado, United States
Presenting Author(s)
Background: ACGME requires pediatric residents to receive training in quality improvement (QI) processes. A needs assessment revealed that our residency program’s curriculum led to few projects utilizing 5 QI Tools (a specific, measurable, applicable, realistic and timely (SMART) aim; key driver diagram (KDD); measurement plan; data display over time; plan-do-study-act (PDSA) cycle) identified as essential to QI methodology.
Objective: Develop, implement and evaluate a QI curriculum for pediatric residents using coaching and experiential learning as a conceptual model.
Design/Methods: We developed a longitudinal curriculum that adhered to Kern’s 6-steps of curriculum development and focused on the Institute for Healthcare Improvement’s Model for Improvement. The curriculum included 5 sessions facilitated by faculty trained in QI methodology. Didactics and small groups allowed for practice and application of tools to active resident projects. Residents had access to 1-on-1 faculty coaching, where progress and barriers were addressed. The curriculum was implemented in December of 2021 for all pediatric residents. Evaluation consisted of: utilization rates for the 5 QI Tools, surveying residents regarding application of QI methodology, and basic interpretative qualitative analysis of open-ended survey questions.
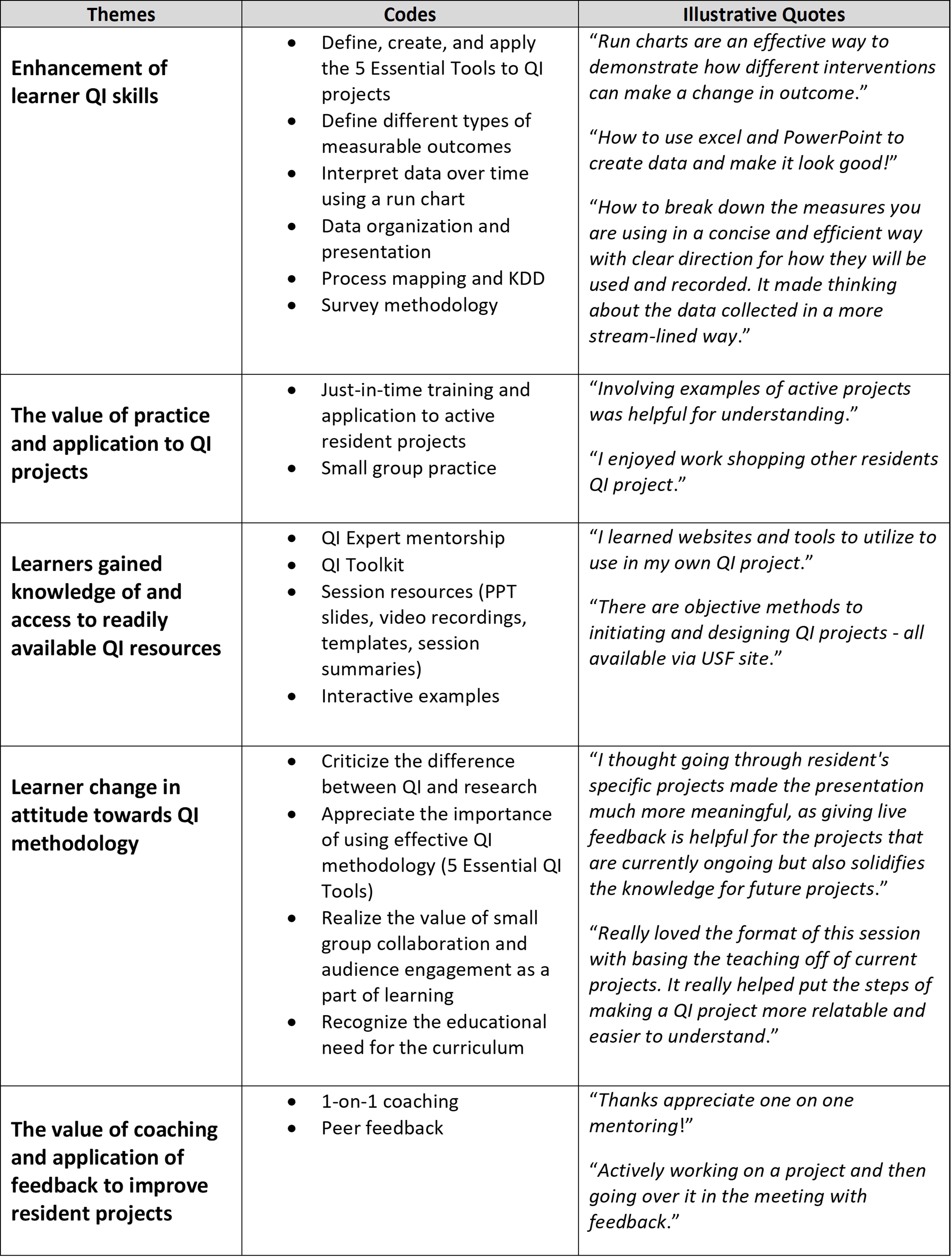
Results: By June of 2022, the completion rate of all 5 learning sessions by pediatric residents was 94% (65% attended live sessions, 35% via recording). After curriculum implementation, a greater percentage of resident QI projects demonstrated improved utilization of the 5 QI Tools: 63% of projects included a SMART aim (vs. 33% at baseline), 75% included a KDD (vs. 20%), 38% involved a measurement plan (vs. 27%), 75% displayed data over time (vs. 53%), 100% used at least one PDSA cycle (vs. 87%). Survey results demonstrated 93% of residents reported being "extremely" or "somewhat likely" to use the 5 QI Tools. Qualitative analysis of open-ended survey questions revealed 5 themes related to the impact of the curriculum: 1) enhancement of QI skills; 2) value of practice and application; 3) knowledge of and access to QI resources; 4) changed attitudes related to QI; 5) value of coaching and application of feedback (Table 1).
Conclusion(s): Our QI curriculum increased resident utilization of essential QI Tools and self-reported improvement in QI skills, knowledge and attitudes. Results highlight the value of feedback and practice of QI tools and applying them to active resident projects. Next steps include evaluation of 1-on-1 coaching through focus groups and more coaching on measurement plan development.