Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 5: Surfactant and NIV 2
681 - Ventilation during nasal intermittent positive pressure ventilation - does rate matter?
Publication Number: 681.443
- OH
Ori Hochwald
director, NICU
Rambam Medical Center, Haifa, Israel
Haifa, Hefa, Israel
Presenting Author(s)
Background:
Nasal intermittent positive pressure ventilation (NIPPV) is commonly used in the NICU. Unlike in the case of invasive ventilation, the effect of increasing or decreasing the set rate on CO2 levels is questionable and not well studied.
Objective:
To examine the change in CO2, when applying NIPPV with either a low or a high rate in stable premature infants.
Design/Methods:
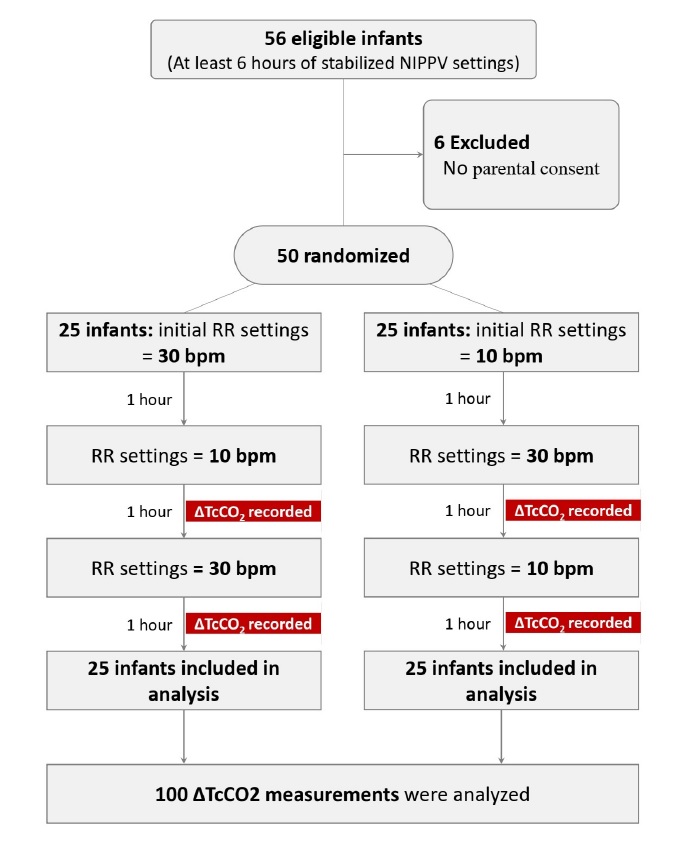
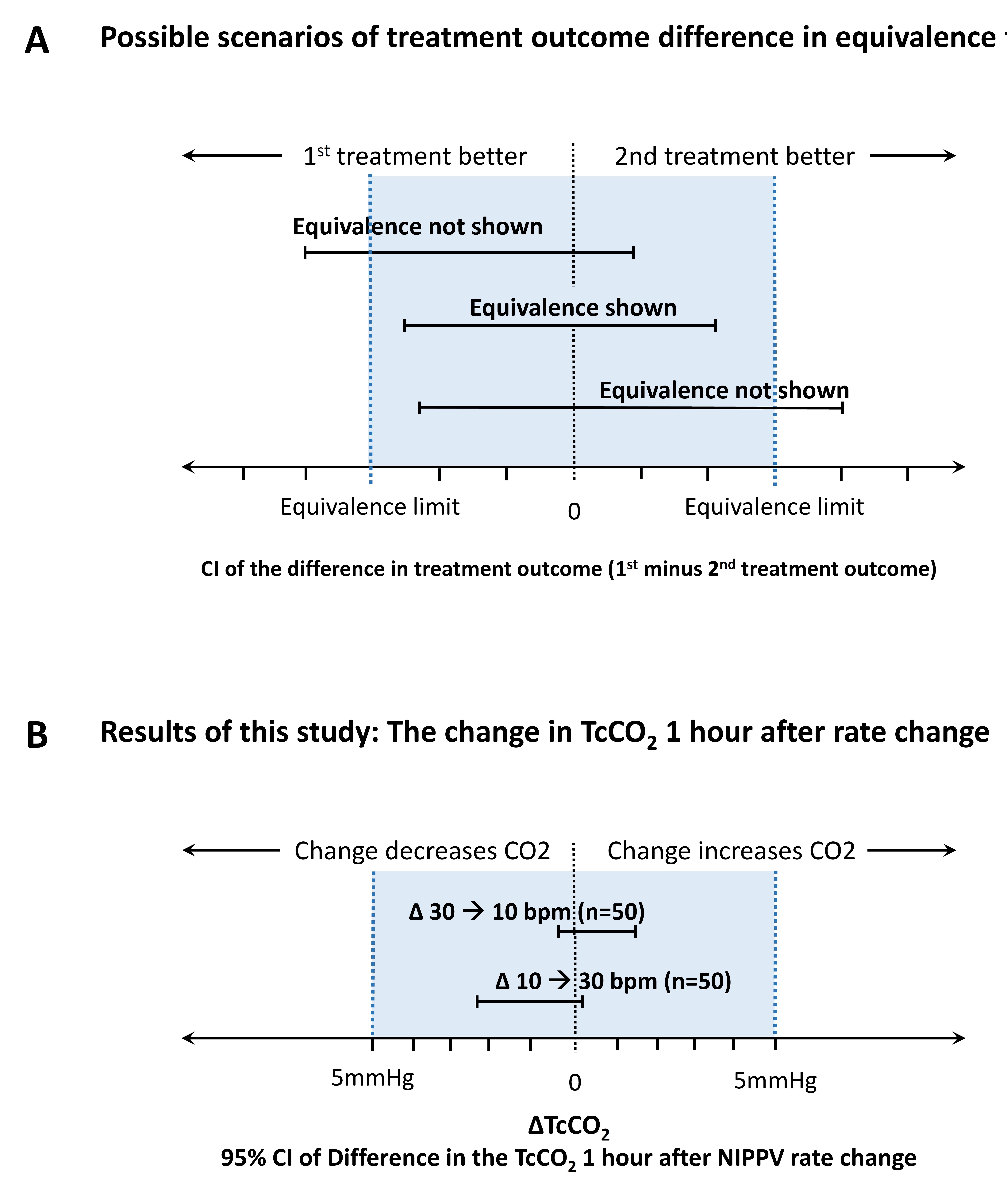
Single center, prospective, controlled, crossover study. Preterm infants on NIPPV were monitored by transcutaneous CO2 monitor (tcCO2) during three consecutive time periods of one hour each on a high (30 bpm) and low (10 bpm) set rate of NIPPV. NIPPV rate was randomly set as high/low, changed to low/high and vice versa. tcCO2 was documented 1 hour after each change. We considered a clinically significant change in CO2 level as 5 mmHg.
Results:
Fifty premature infants (mean±SD: 28.3±2.4 weeks’ gestation) were enrolled. Each infant had two rate changes; therefore, a hundred rate changes were studied. The mean change in tcCO2, i.e., ΔtcCO2 (95% confidence-interval), was -1.1 (-2.3 to 0.1) mmHg for increasing rate from low to high, and 0.46 (-0.49 to 1.41) mmHg for decreasing rate from high to low (figure, B). There was no significant change in spontaneous respiratory rate, FiO2, desaturations, apnea and bradycardia events, but mean airway pressure and oxygen spO2 increased (p< 0.05).
Conclusion(s):
Our study found that multiplying or dividing the rate setting by three, did not significantly change the tcCO2 readings an hour after the change, in stable preterm infants supported by NIPPV. These findings could affect the management of ventilation setting of NIPPV in premature infants, but should be confirmed in future studies also in unstable premature infants.