Neonatal Infectious Diseases/Immunology
Neonatal Infectious Diseases/Immunology 6
459 - Applying the Sepsis Risk Score to Asymptomatic Neonates with Complex Congenital Anomalies
Publication Number: 459.432
- LF
Leigh M. Finnegan, MD (she/her/hers)
Attending Physician
Children's Hospital of Los Angeles
Los Angeles, California, United States
Presenting Author(s)
Background:
Early-onset sepsis (EOS) is associated with significant neonatal morbidity and mortality. However, in the current era EOS rates are low, and neonatal antibiotic exposure is known to be associated with adverse long-term outcomes. The Sepsis Risk Score (SRS) is a validated tool to guide antibiotic initiation for EOS based on sepsis risk for infants born at ≥34 weeks’ gestation. The SRS is rarely used in infants with complex congenital anomalies, whose underlying conditions may lead to clinical instability that is indistinguishable from infection.
Objective:
To measure rates of early antibiotic initiation in asymptomatic infants with congenital anomalies born in the Children's Hospital of Philadelphia's Special Delivery Unit (SDU) at ≥34 weeks' gestation with low SRS at delivery.
Design/Methods:
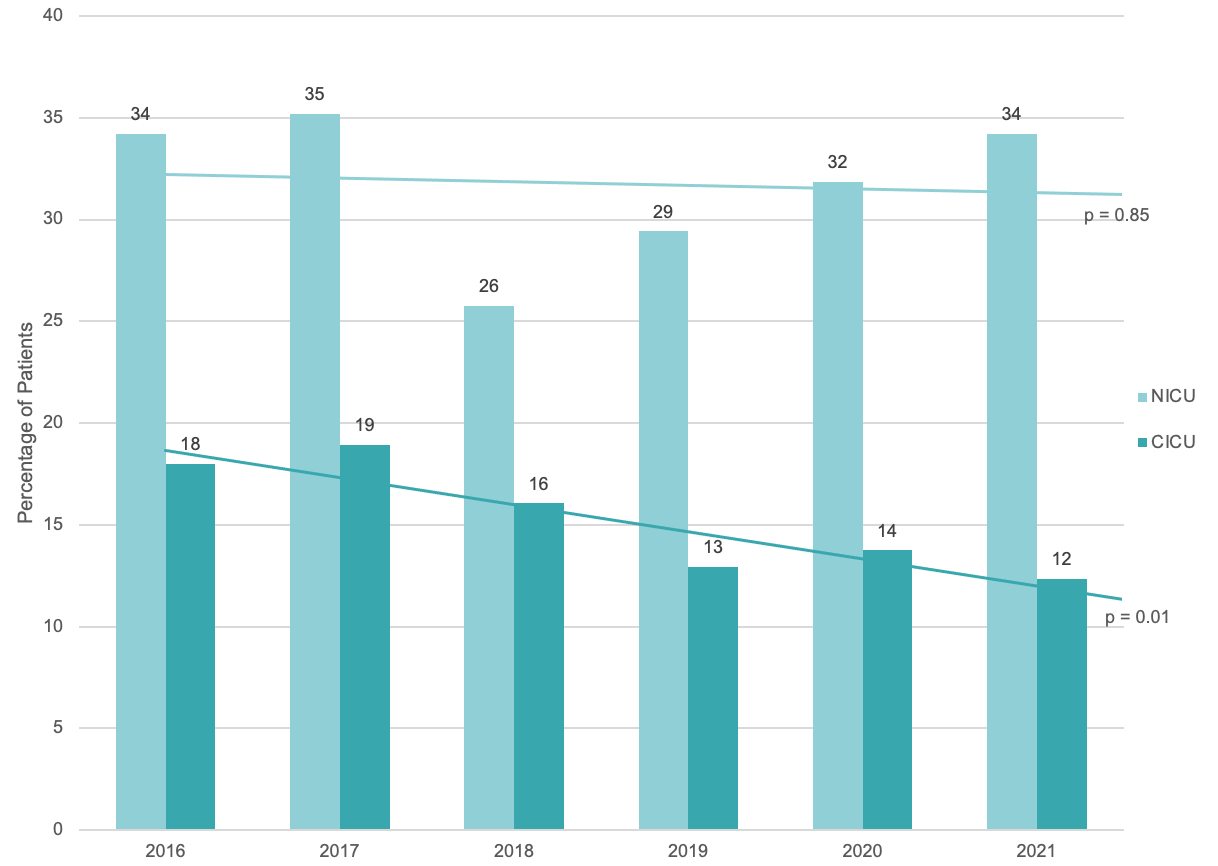
Retrospective study of infants born in the SDU from 10/2015-12/2021 and admitted to the neonatal (NICU) or cardiac (CICU) intensive care unit. SRS was calculated with Neonatal Early Onset Sepsis Calculator formula using infant and maternal data. We analyzed rates of early antibiotic initiation (within 72h of life) in the subgroup of infants with low SRS (< 0.65) without markers of clinical illness (defined by use of pressors, steroids, invasive ventilation, or fever in the first 72h). Analysis included summary statistics, Chi-squared analysis, and Wilcoxon rank-sum. We calculated how many infants without clinical illness could potentially have been spared antibiotic exposure, and examined trends by year, admission unit and underlying diagnosis.
Results:
From 10/2015-12/2021, 2408 patients were born in the SDU who met inclusion criteria. Of those patients, 1475 had low SRS and no markers of clinical illness within the first 72h (61%). Of those patients, 381 (26%) received antibiotics within the first 72h (Fig. 1). Rates differed by unit of admission (Fig. 2) and by congenital diagnosis (Table 1). Rates of antibiotic use in the CICU decreased over time (p=0.01), but did not significantly change in the NICU (p=0.85). In the subgroup with low SRS and low illness severity, early antibiotic exposure was associated with longer length of stay (median 29.1d vs 19.7d, p< 0.01), but no difference in mortality was observed at 7d (p=0.39) or 28d (p=0.27).
Conclusion(s):
Applying the SRS to asymptomatic patients with complex congenital anomalies could result in a decrease in antibiotic exposure. Further analysis is required to understand factors influencing decision-making about antibiotic initiation in infants with complex congenital anomalies, as well as the impact of excess early antibiotic exposure on outcomes in this cohort. 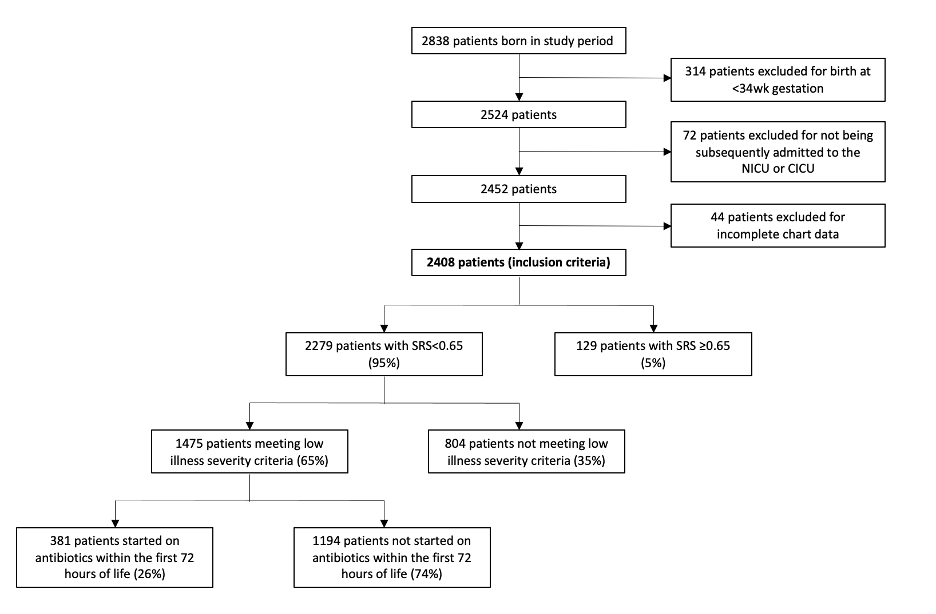
.png)
