Cardiology
Cardiology 3
717 - Parental Perspectives on Pediatric Heart Transplantation: A Qualitative Needs Assessment
Publication Number: 717.4

Katherine Aschheim, MD, MSc (she/her/hers)
Resident Physician
NewYork-Presbyterian Morgan Stanley Children's Hospital
New YorK, New York, United States
Presenting Author(s)
Background:
Understanding the pediatric caregiver experience of heart transplantation is crucial to providing optimal medical care, though few studies focus on this perspective.
Objective: To explore parents’ experiences during the heart transplantation process in order to identify best practices and opportunities for improvement within our heart failure program.
Design/Methods: English-speaking parents of children who received heart transplantations at a quaternary care hospital in New York City from May 2022 to November 2022 were eligible for enrollment. A member of the heart failure team recruited participants for the study. Interviews were semi-structured and in-depth, approximately 30-45 minutes in duration. Data were coded independently by 3 investigators to generate a codebook that was iteratively revised. Codes were organized into common themes using the constant comparative method. All analyses were performed using nVivo, a qualitative analysis software package. A multiple-choice demographic survey was also administered before the interviews.
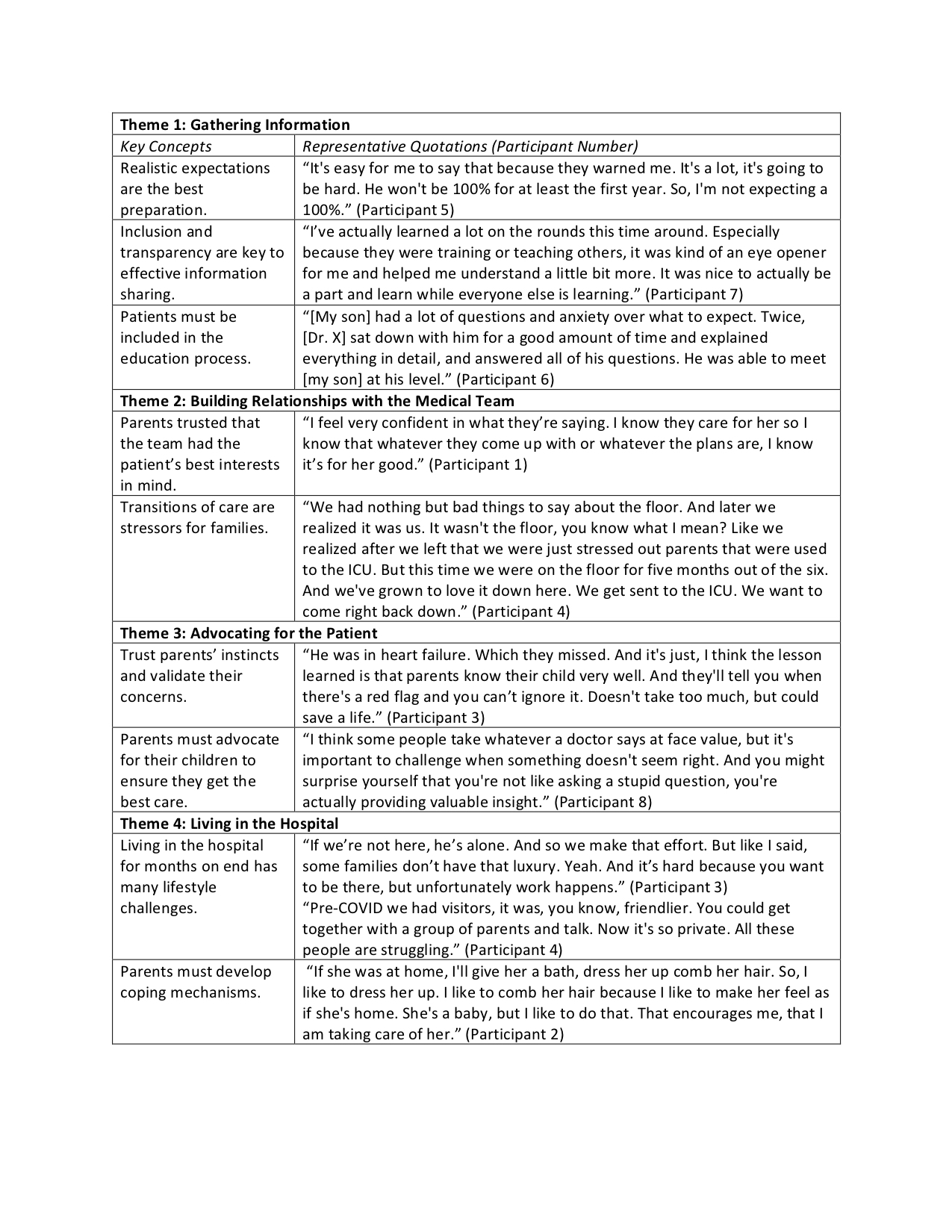
Results: We conducted 8 interviews with parents of children who underwent heart transplantation. The participants were mostly mothers of school-aged children from diverse racial and ethnic backgrounds (Table 1). Participants’ experiences were categorized in 4 major themes: 1) gathering information – to navigate the complexity of their child’s care; 2) building relationships with the medical team – despite obstacles to trust such as frequent transitions; 3) advocating for the patient – both their medical care and well-being; and 4) living in the hospital – especially coping with the challenges that arise during a prolonged admission (Table 2). Through their discussion of these themes, participants identified best practices and unmet needs within our transplant program. Best practices included realistic expectation setting, inclusion in rounds, transparency with medical decision making, and the establishment of a trusting relationship with providers. Unmet needs included inviting patients into medical discussions, consistent communication from all members of the team, validation of parental perspectives, and the ability to connect with other families with similar experiences.
Conclusion(s):
This needs assessment generated valuable feedback for our heart failure program that could be used as the basis for future quality improvement initiatives. If further study corroborates these findings, they may also help other centers who wish to improve patient and caregiver experiences in their transplantation programs. .jpg)