Cardiology
Cardiology 3
715 - Markers of growth and nutrition in children with acquired chylothorax post congenital heart disease surgery
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 715
Publication Number: 715.4
Publication Number: 715.4
Kevin N. Marzotto, Tulane University School of Medicine, New Orleans, LA, United States; Karin Videlefsky, Tulane University School of Medicine, New Orleans, LA, United States; Meghan Howell, Tulane University School of Medicine, New Orleans, LA, United States; Frank Pigula, Louisiana State University School of Medicine in New Orleans, new orleans, LA, United States; Thomas R. Kimball, Louisiana State University School of Medicine in New Orleans, New Orleans, LA, United States; Kurt Piggott, University of Central Florida College of Medicine, Orlando, FL, United States
.jpg)
Kevin N. Marzotto, BA (he/him/his)
Medical Student
Tulane University School of Medicine
New Orleans, Louisiana, United States
Presenting Author(s)
Background: Acquired chylothorax (leakage of chylous fluid into pleural space) is an established complication of congenital heart disease (CHD) surgery, affecting 4-9% of patients. CHD increases risk of failure to thrive, with chylothorax imposing additional risk. Following our systematic review, a paucity of studies were found to investigate growth and nutritional consequences of chylothorax.
Objective: We conducted a retrospective chart review to ascertain quantitative markers of nutrition and growth in children affected by chylothorax following CHD surgery between 2018-2022 compared to controls.
Design/Methods: We utilized electronic medical record system, EPIC, at Children’s Hospital, New Orleans, targeting subjects < 18 years old who underwent CHD surgery between 2018 and 2022 and developed a subsequent chylothorax. Study subjects were identified using ICD-10 codes (J94.0, I89.8, and J90.0). Each chylothorax case (n=20) was matched by procedure type and age to a control with no chylothorax (n=20). Data was recorded in REDCap and analyzed using SPSS.
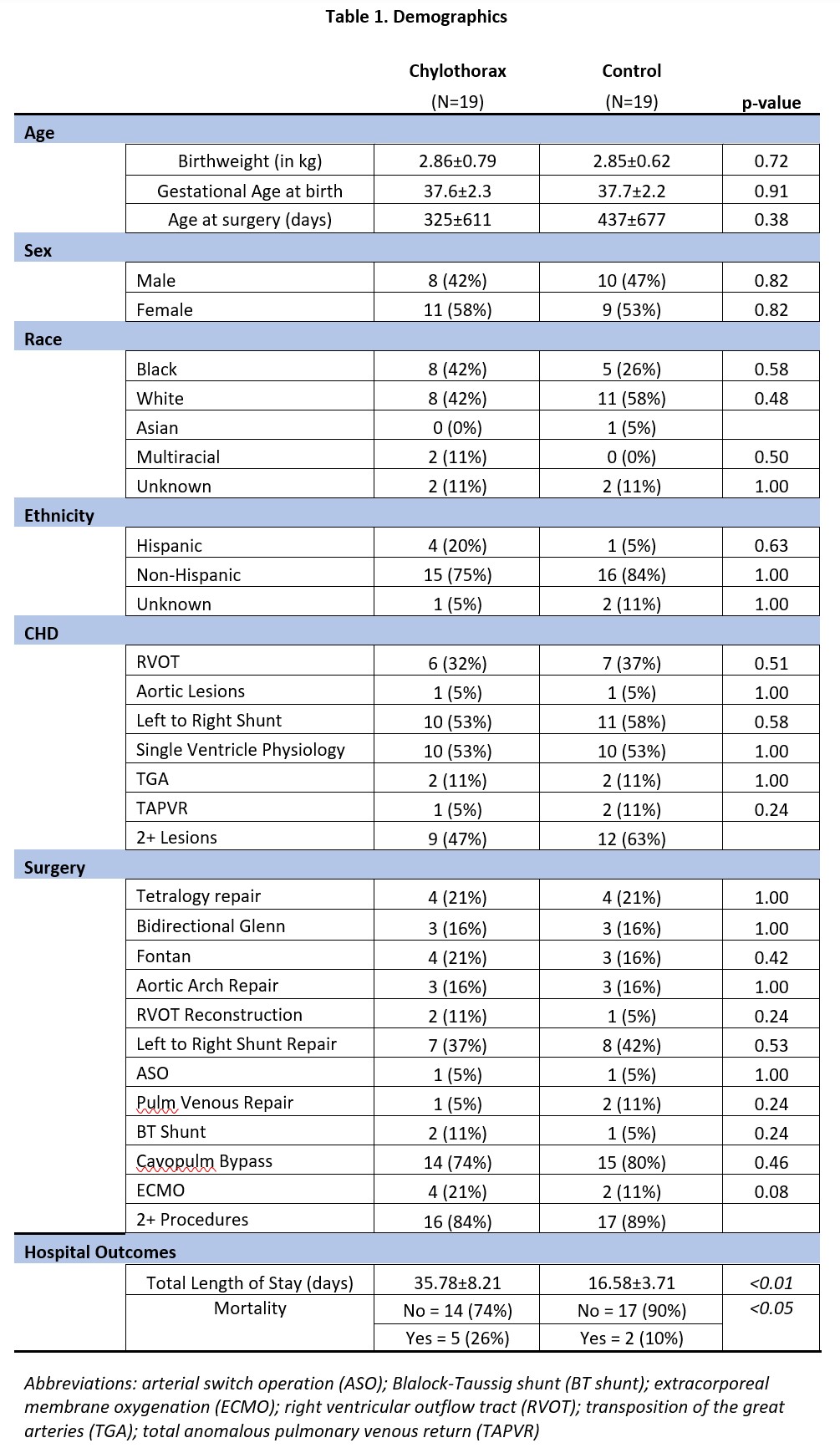
Results: Demographics are represented in Table 1. One case and one control were removed as outliers due to growth velocity, yielding 19 total matched pairs. Descriptive statistics of our hospital, growth and nutritional variables are outlined in Table 2. When comparing cases to controls via student’s t-test, there was no difference in Growth Velocity (p=0.12), Weight Change (Operation to Discharge) (p=0.95), Weight Change (Admission to Discharge) (p=0.35), Z-Score Change (Operation to Discharge) (p=0.90), Z-Score Change (Admission to Discharge) (p=0.21), Serum Protein (p=0.88) and Serum Albumin (p=0.82). Serum Pre-Albumin and Serum Triglycerides could not be compared due to excessive missing values. Among cases alone, linear regression demonstrated no significant association between Maximum Chylous Output with Growth Velocity (p=0.91), Weight Change (Operation to Discharge) (p=0.15), and Weight Change (Admission to Discharge) (p=0.98). Mann Whitney U Test showed no statistical change in Chylous Triglyceride Level in cases with No Weight Gain/Loss compared to subjects with Weight Gain over the hospital course (p=0.733).
Conclusion(s): Compared to controls, cases did not have statistically significant markers of growth or nutrition. For cases of chylothorax, maximum chylous output and chylous triglyceride level were not associated with markers of growth and nutrition in CHD patients with chylothorax. Limitations include our small sample size; thus, multisite data collection and analysis is required to better ascertain clinical impact and guide clinical practice.
.jpg)
