Medical Education: Resident
Medical Education 13: Resident 4
477 - Pediatric Emergency Response Simulation Curriculum for Residents
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 477
Publication Number: 477.421
Publication Number: 477.421
Rachael A. Herriman, Comer Children's Hospital at University of Chicago Medical Center, Chicago, IL, United States; Priti Jani, Comer Children's Hospital at University of Chicago Medical Center, Chicago, IL, United States; Anu Elangovan, Comer Children's Hospital at University of Chicago Medical Center, Chicago, IL, United States; Nehal Patel, Comer Children's Hospital at University of Chicago Medical Center, Chicago, IL, United States; Brett K. Palama, University of Chicago, Chicago, IL, United States

Rachael A. Herriman, MD (she/her/hers)
PGY3
Comer Children's Hospital at University of Chicago Medical Center
Chicago, Illinois, United States
Presenting Author(s)
Background: Pediatric clinical deterioration outside the intensive care unit is associated with increased morbidity and mortality. Rapid response team (PET) events rely on effective communication for patient safety. For pediatric residents at our tertiary care hospital, no formal training exists for PET events. Previous studies have utilized simulation to improve communication in rapid responses through SBAR (Situation, Background, Assessment, Recommendation) and ABC (Airway, Breathing, Circulation). While simulation-based training is highly effective in improving non-emergent handoff skills, research on ideal training during emergent handoffs is limited.
Objective: To evaluate the efficacy of a simulation-based curriculum in improving handoffs during pediatric emergency response events.
Design/Methods: This study incorporates novel aspects of real-time training, peer-to-peer rapid feedback and deliberate practice to improve communication, confidence and understanding of the value of PET handoffs. 1 month prior to their pediatric inpatient rotation, pediatric and med-peds residents PGY1-PGY4 (N=10) participated in a simulation-based curriculum. Following initial audio recorded simulation, residents completed didactics and practiced 2 PET handoffs with peer feedback. A final recording simulation was then completed. Pre- and post-curriculum surveys evaluated PET knowledge and prior experiences. Simulation-based assessments evaluated handoff content, structure and efficiency using a previously published pediatric communication scoring tool (total maximum score=10). Statistical evaluation included Pearson correlation coefficient and T-tests.
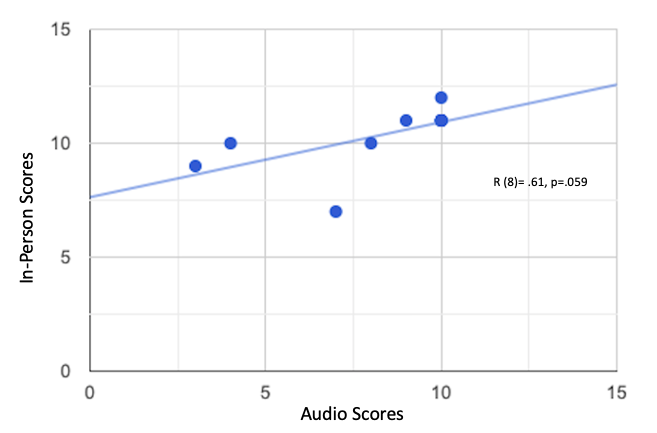
Results: 50% of participants were first year residents, 93.8% were categorical pediatric trainees. 62.5% of participants had never led a PET. Prior to training, 50% had no or low confidence to lead a PET. Following the curriculum, 70% had moderate confidence, 20% had high confidence and 0% had no or low confidence to lead a PET. Mean total score of hand-offs significantly improved [pre-training 5.2 versus post-training 8.1 (p< .05)]. Mention of ABC improved significantly (p< .05). Overall score of in-person versus audio recorded rating showed a moderately strong correlation (p=.059).
Conclusion(s): Study results provide further insight into the ideal training methodology for emergent handoffs and corroborate previous ABC-SBAR studies. This pilot study, with goal N=50, will extend to the full pediatric residency and become a permanent training component at our institution to improve patient outcomes in settings of acute decompensation.
.png)