Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 8
572 - Racial Differences in Insurance Classification of Non-Emergent ED Visits
Publication Number: 572.412

Alexander Pomerantz, MD, MPP (he/him/his)
Resident Physician in Pediatrics
Boston Children's Hospital/Boston Medical Center
Boston, Massachusetts, United States
Presenting Author(s)
Background:
Numerous state Medicaid programs and commercial insurers have
enacted policies to discourage unnecessary emergency department (ED) visits by reducing or
denying reimbursement for visits retrospectively classified as non-emergent based on claims
algorithms. Recognizing that low-income Black and Hispanic children often experience worse
access to primary care services needed to prevent some ED visits, we hypothesized these policies
may manifest in racial or ethnic differences in reimbursement.
Objective:
We sought to examine potential racial and ethnic differences in a commonly used insurance algorithm and model the potential impacts on clinician reimbursement by applying one current state Medicaid policy.
Design/Methods:
We performed a retrospective cohort study of 8.4 million outpatient pediatric ED
visits across 9-12 de-identified states in the MarketScan Medicaid database between 2016-2019.
We applied a widely utilized diagnosis-based claims algorithm to identify non-emergent ED
visits. We then utilized a reimbursement reduction policy employed by one state Medicaid
agency to simulate potential impacts on expected per-visit professional reimbursement, by race
and ethnicity, across the entire cohort.
Results:
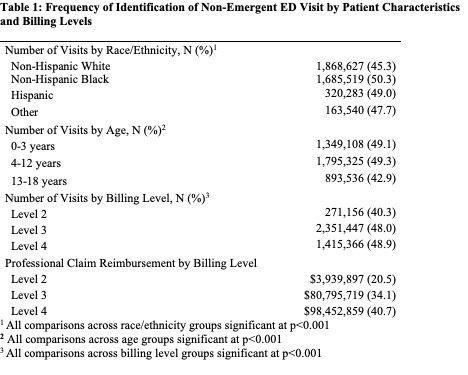
The algorithm identified 47% of ED visits as non-emergent and subject to
reimbursement reduction. More visits by Black children (50%) and Hispanic children (49%)
were algorithmically identified as non-emergent when compared with White children (45%),
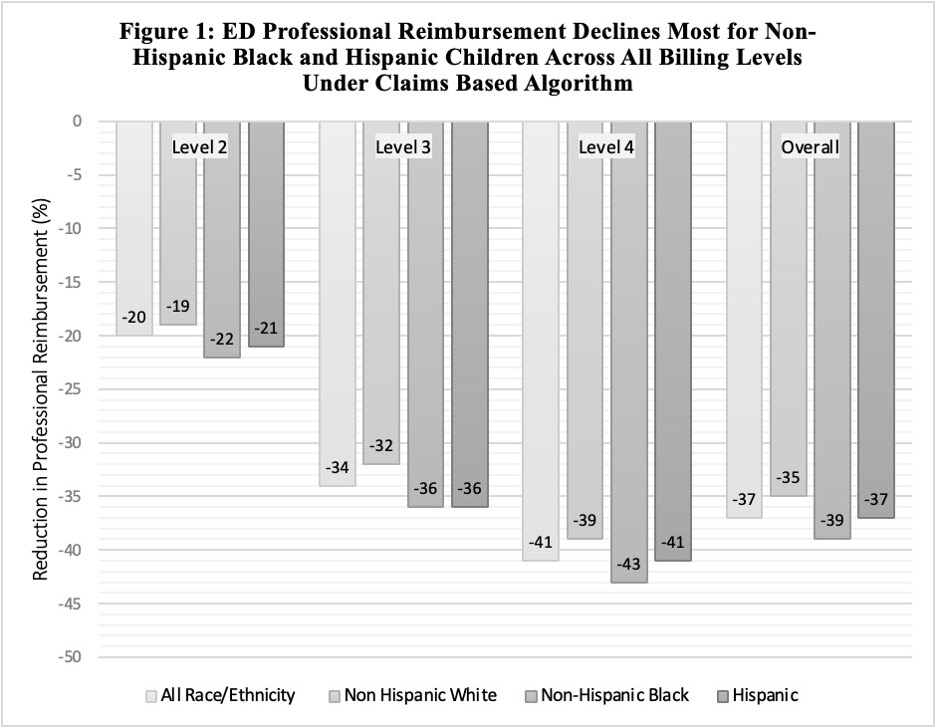
p< .001 (Table 1). Application of the algorithm’s reimbursement reduction would reduce ED
reimbursement by 37%. The relative decrease was greater for ED visits for Black children
(-39%) and Hispanic children (-37%) than for White children (-35%) and was consistent across
original billing levels (Figure 1). Modeling the impact of the reimbursement reductions resulted
in expected per-visit reimbursement that was 6% lower for visits for Black children and 3%
lower for visits for Hispanic children, relative to White children.
Conclusion(s):
Algorithmic approaches for classifying pediatric ED visits using diagnosis codes
may disproportionately identify more visits by Black and Hispanic children as non-emergent.
Insurers applying financial adjustments based on such algorithms risk creating differences in
clinician reimbursement based on the racial and ethnic composition of the patient population.
Disparate reimbursement may exacerbate structural barriers to care and impede investments that
may influence quality of care.