Hospital Medicine: Clinical
Hospital Medicine 7
774 - Keeping Score - Outcomes of Universal Delirium Screening at a Tertiary Care Children's Hospital
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 774
Publication Number: 774.416
Publication Number: 774.416
Madalyn Gibson-Williams, University of Connecticut School of Medicine, West Hartford, CT, United States; Hayley Wolfgruber, University of Connecticut School of Medicine, Hartford, CT, United States; Hareem Park, Hasbro Children's Hospital at Rhode Island Hospital, Providence, RI, United States

Madalyn Gibson-Williams (she/her/hers)
Medical Student
University of Connecticut School of Medicine
West Hartford, Connecticut, United States
Presenting Author(s)
Background: Delirium is a neuropsychiatric condition characterized by dysfunction of behavior, cognition, and awareness. It is associated with increased length of stay and time on ventilator support. The prevalence of delirium in pediatric critical care patients is between 12% and 65%. There are few studies in the non-critical care population. Early detection and appropriate intervention may improve patient outcomes.
Objective: Determine the prevalence of delirium in pediatric non-critical care inpatient settings and the impact of delirium screening on patient care.
Design/Methods: A clinical pathway for delirium was implemented at Connecticut Children’s. Beginning in April 2019, all inpatients were screened for delirium with the Cornell Assessment of Pediatric Delirium (CAPD). Scores of 9 or greater were considered positive. The authors performed chart review to investigate the prevalence of true delirium in patient encounters with positive screens. The diagnosis of delirium was confirmed by psychiatry evaluation when completed or by clinical description as agreed upon by two reviewers with inter-rater reliability. Additional chart review investigated changes in management associated with positive screens.
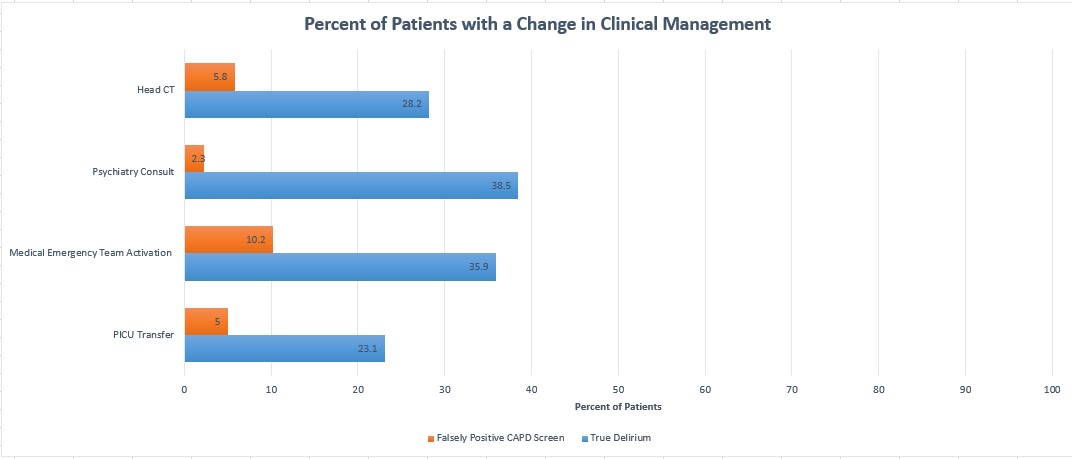
Results: From April 2019 to June 2020, 502 of 9,223 patient encounters had a positive screen (5.4%). Of those with positive screens, 71 (14%; 0.8% of all patient encounters) were determined to have true delirium, while 431 (86%) were determined to have falsely positive scores. 72% of patients with positive screens had a developmental delay while 17% were less than 6 months old. Based on chart review, 304 (71%) falsely positive scores were determined to be secondary to difficulty in scoring patients with developmental delay and 46 (11%) due to young age. Of patients with true delirium, 23% had a PICU transfer, 36% had a medical emergency team activation, 39% underwent psychiatric evaluation, and 28% had a head CT. This is in contrast to 5%, 10%, 2%, and 6% respectively in those with falsely positive scores.
Conclusion(s): The prevalence of delirium was lower in non-critical care inpatient settings. Those with true delirium were more likely to have a change in management. Patients with developmental delay and infants were more difficult to score accurately reflected by higher rates of falsely positive screens. The CAPD may require more training to be valid in these patients. Due to the lower prevalence of delirium in the non-critical care patients, focused screening for high-risk patients may be more effective.