Medical Education: Resident
Medical Education 15: Resident 6
503 - Assessing pediatric and family residents' knowledge in food allergy: Initial report of a 2-phase educational intervention in two New York hospitals
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 503
Publication Number: 503.423
Publication Number: 503.423
Crhistian Toribio-Dionicio, New York Medical College, Metropolitan Hospital Center, New York, NY, United States; Nizar Tangour, New York Medical College, New York, NY, United States; Gabriel Sraha, Saint Josephs Medical Center, Yonkers, NY, United States; Ruth Vela-Sosa, New York Medical College, New York, NY, United States; Juhee Lee, New York Medical College, New York, NY, United States; Arpit Gupta, New York Medical College/Metropolitan Hospital Center, New York, NY, United States

Crhistian Toribio-Dionicio, MD (he/him/his)
Pediatric Resident
New York Medical College, Metropolitan Hospital Center
New York, New York, United States
Presenting Author(s)
Background: The prevalence of food allergy is increasing and affects 8% of the pediatric population. The severity of symptoms is unpredictable, ranging from mild reactions to anaphylaxis. Management includes avoidance of food allergens and immediate intervention after accidental exposure.
Previous studies found that allergists did not evaluate 67% of children with physician-documented food allergies due to a lack of a referral. Also, fewer than 30% of pediatricians felt comfortable caring for children with food allergies and interpreting allergy laboratory tests. Therefore, given the impact on children's quality of life and the possibility of a fatal outcome, primary care physicians play an essential role in caring for children with food allergies.
Objective: To assess the level of knowledge of food allergy in pediatric and family medicine residents in Metropolitan Hospital Center and Saint Joseph's Medical Center, respectively.
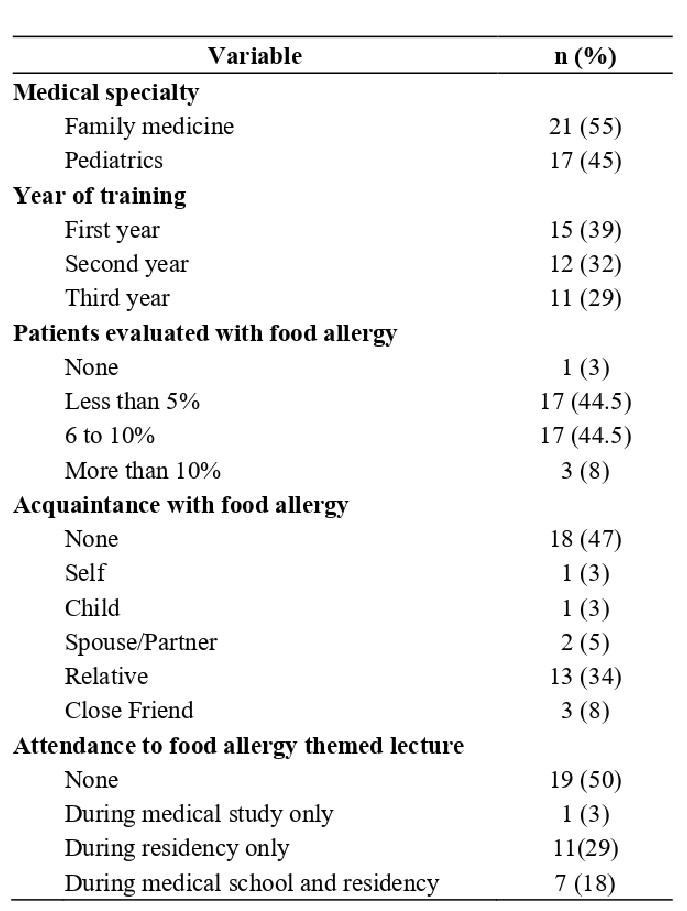
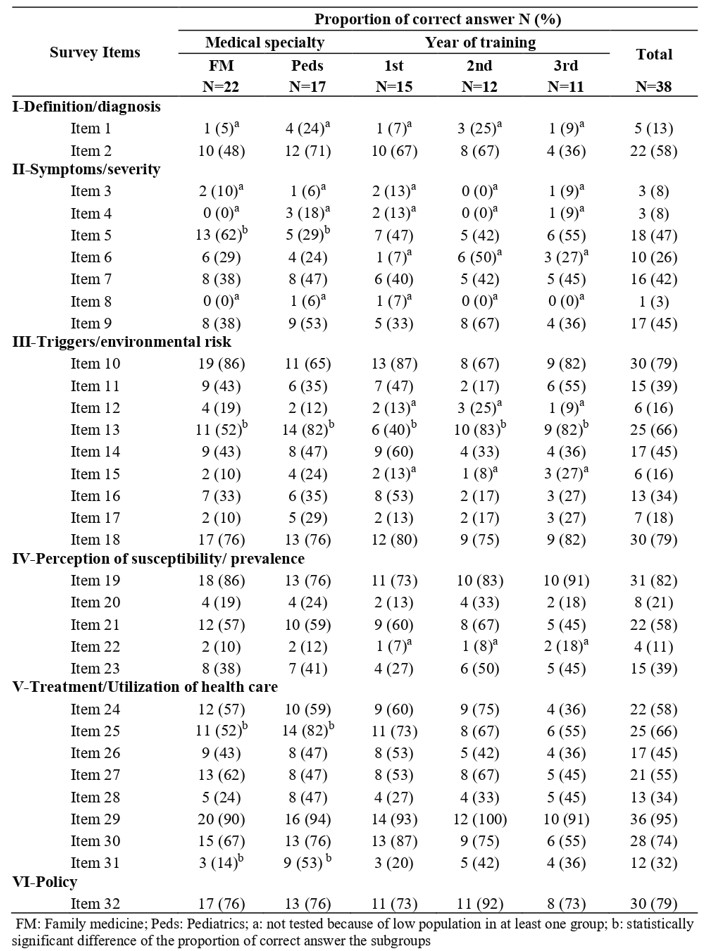
Design/Methods: Participation was offered to pediatric and family medicine residents between August and November 2022. They answered the Chicago Food Allergy Research Survey for Primary Care questionnaire to assess their level of knowledge. Items were divided into 6 subcategories. Demographic variables included specialty, year of training, and age. A score was calculated based on the proportion of correct answers for knowledge items and their subcategories for each resident group. Student T-test, Welch T-test, one-way ANOVA, Chi-square test, and Fisher exact test were used when appropriate.
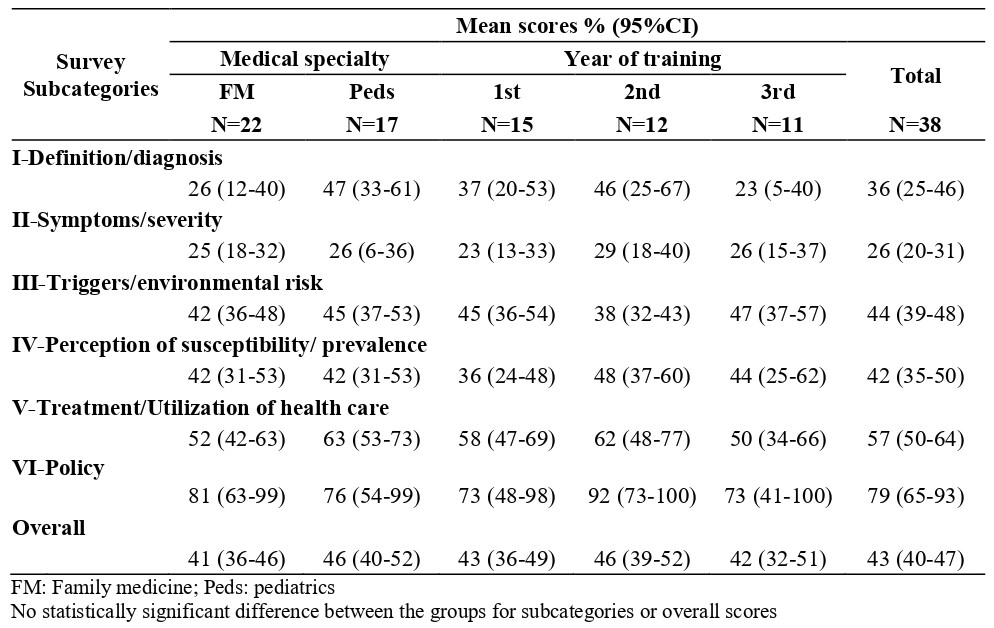
Results: Thirty-eight residents were included in the study. Eighteen participants (45%) were pediatric residents. Fifty percent of residents had a lecture during medical school and/or residency. The mean score of level of knowledge was 43% (95%CI: 40-47%), and the mean scores for pediatric and family medicine residents were 46% (95%CI: 40-52%) and 41% (95%IC: 36-46%), respectively. No significant statistical difference in the mean scores was found between subspecialties or levels of training. The highest scores were for the policy subcategory and the lowest for the symptoms and severity subcategory. Overall, subcategories' mean scores ranged from 26% to 79%, with the same tendencies in specialty and level of training subgroups. No significant statistical difference in subcategories scores was found between subspecialties scores or level of training.
Conclusion(s): Both resident groups had low food allergy knowledge. Moreover, the absence of differences in scores among the levels of training emphasizes the need for subsequent training sessions focusing on current diagnoses and management guidelines.