Medical Education: Resident
Medical Education 15: Resident 6
508 - Implementation of a Pilot Curriculum to Increase Pediatric Resident Comfort and Practice of Motivational Interviewing
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 508
Publication Number: 508.423
Publication Number: 508.423
Austin Lewis, Medical University of South Carolina, Charleston, SC, United States; Georgia Lydon, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Christine SanGiovanni, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Kathleen C. Head, Medical University of South Carolina, Charleston, SC, United States

Austin Lewis, MD (he/him/his)
Resident - Internal Medicine and Pediatrics
Medical University of South Carolina
Charleston, South Carolina, United States
Presenting Author(s)
Background: Use of motivational interviewing (MI) in the clinical setting improves patient health outcomes. MI training is not required in most residency programs. Core elements of MI include collaboration, evoking, autonomy and compassion and creating SMART goals.
Objective: This pilot aimed to better understand an academic institution’s pediatric residents’ comfort with and use of MI, and to implement a curriculum in MI based on needs.
Design/Methods: MUSC pediatrics residents were included (54). A Likert-style pre-intervention survey was collected to assess resident frequency of MI use and comfort using MI. Answers were scaled from 1(never) to 5(all the time). Direct observations of clinical encounters were performed using a standardized grading rubric along with interactive educational interventions. These interventions were delivered in three sessions (two 15-minute didactics and one 45-minute grand rounds). Identical surveys and direct observations were completed after intervention. Data was analyzed in Microsoft Excel, using unpaired T-test.
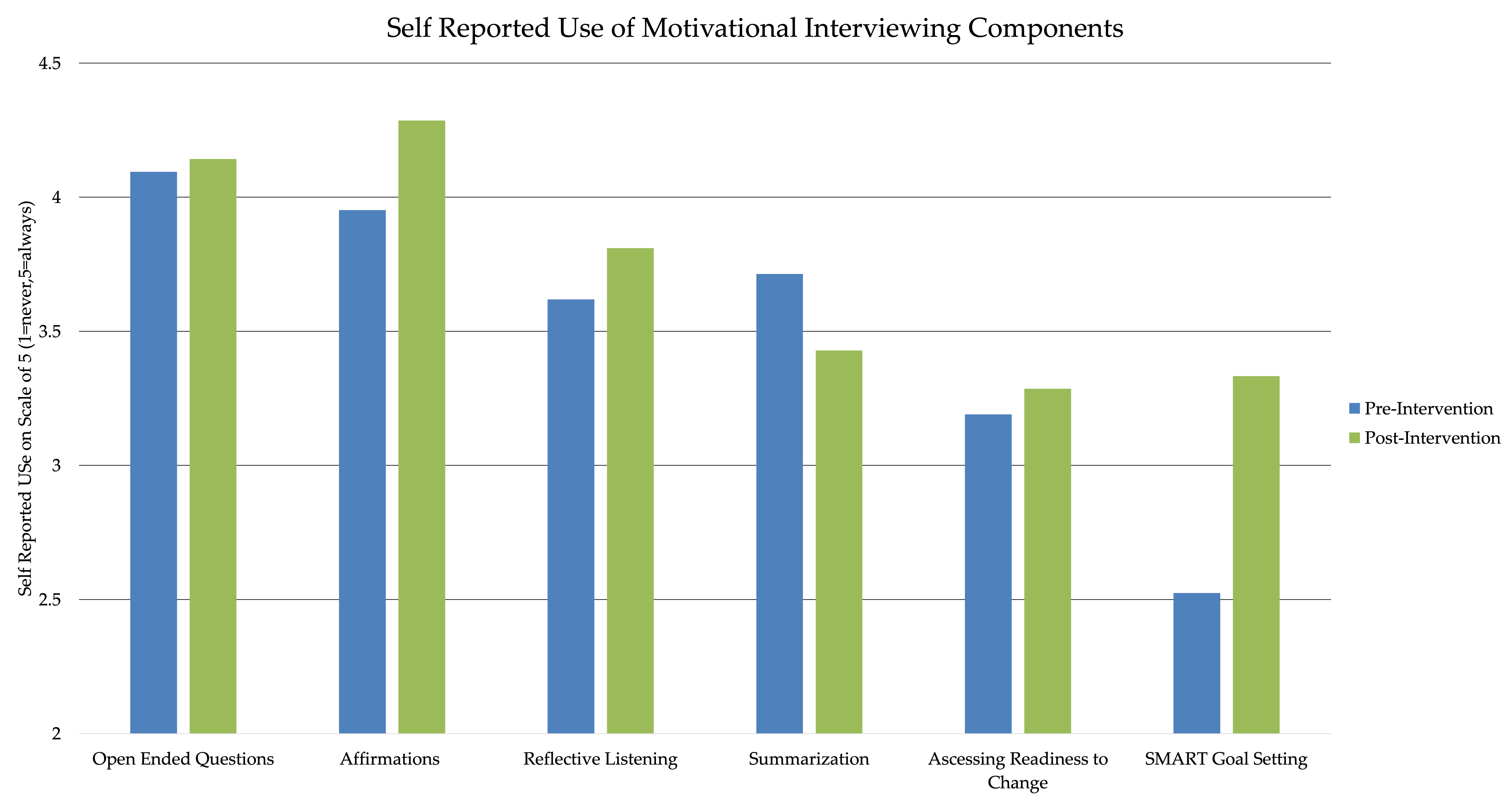
Results: 10 pre-intervention observations were performed. Most residents made appropriate use of open-ended questions during encounters but endorsed difficulty assessing patient readiness for change. Residents often gave medical advice immediately, rather than allowing for patient-led change.
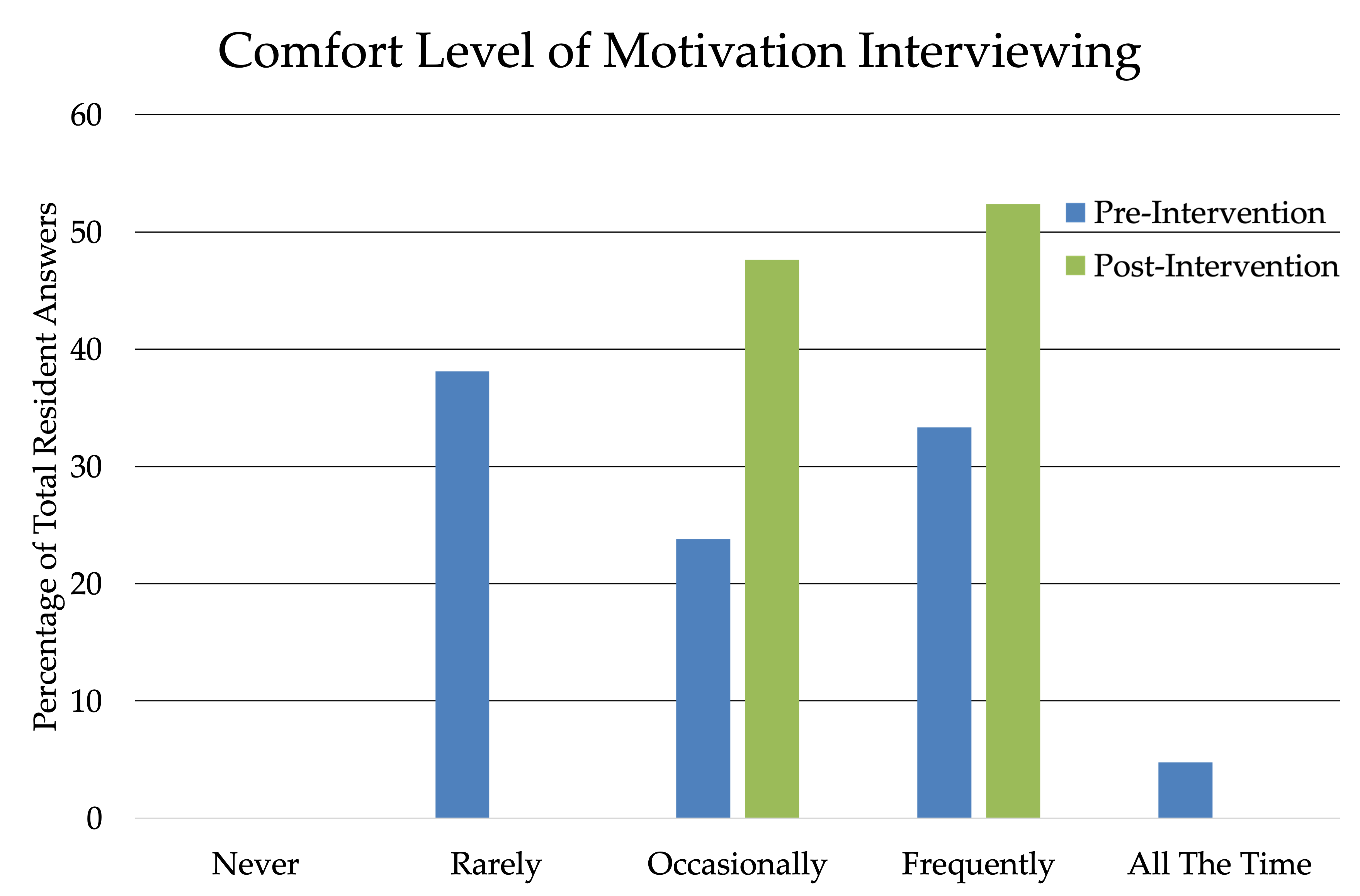
35 pre-intervention surveys were completed. Residents rated frequency of MI implementation and comfort using MI at an average of 3.33 and 3.06 out of 5, respectively.
35 post-intervention surveys showed that residents' overall scores for frequency of MI implementation and comfort using MI had increased to 3.58 and 3.40, respectively (p >.05).
Conclusion(s): Resident participation was associated with increased frequency of use and comfort using MI in clinical encounters, even though not statistically significant. There was also increased use of individual MI components. Prior to the intervention, the most underused component of MI was creation of a SMART goals, which is the ultimate goal of MI. After intervention, resident use and comfort in making SMART goals with patients significantly increased. Even small introductions like the intervention in this study can increase resident comfort and use. Literature suggests experiential learning in MI, like the direct observations included in this pilot, produces more favorable outcomes. Next steps include performing more post-intervention direct observations to obtain objective results, as well as creating a sustainable curriculum including continuing education for faculty to help reinforce resident skills in MI.
.png)