Emergency Medicine: All Areas
Emergency Medicine 13
360 - Contributions of Social Determinant of Health to Risk of Asthma Hospitalization after Treatment in the Emergency Department
Publication Number: 360.404

Michael D. Johnson, MD MS (he/him/his)
Associate Professor of Pediatrics
University of Utah School of Medicine
Salt Lake City, Utah, United States
Presenting Author(s)
Background:
Children with asthma experience disparities by race, ethnicity, and socioeconomic status in the care they receive in emergency departments (EDs). Prior study of the underlying mechanisms of these disparities relied on datasets that lacked detail, were derived from limited populations, or were gathered decades ago.
The Child Opportunity Index (COI) is a regional measure of social determinants of health (SDoH) associated with population-level asthma outcomes. The Pediatric Emergency Care Applied Research Network (PECARN) Registry compiles detailed electronic health record (EHR) data including severity-related factors and SDoH from the EDs of ten children’s hospitals and three affiliated community hospitals.
Objective:
Our aim is to combine the SDoH represented by the COI with the detailed clinical information of the PECARN Registry to derive a prognostic model of hospitalization after ED treatment for asthma that quantifies the contribution of SDoH to disparities in hospitalization.
Design/Methods:
Retrospective cohort study of all children 2-17 years old who visited a PECARN Registry site for acute asthma over four years. The primary outcome was hospitalization. COI was assigned based on zip code of the subject's address in the EHR. Severity measures included presenting vital signs and asthma score severity, as well as triage category, presentation during COVID, and history of hospitalization for asthma in the prior 12 months. Statistical analysis included univariate and multivariable regression models. To quantify the contribution of SDoH to predicting admission, the change in area under the curve (AUC) was compared for models with and without SDoH variables.
Results:
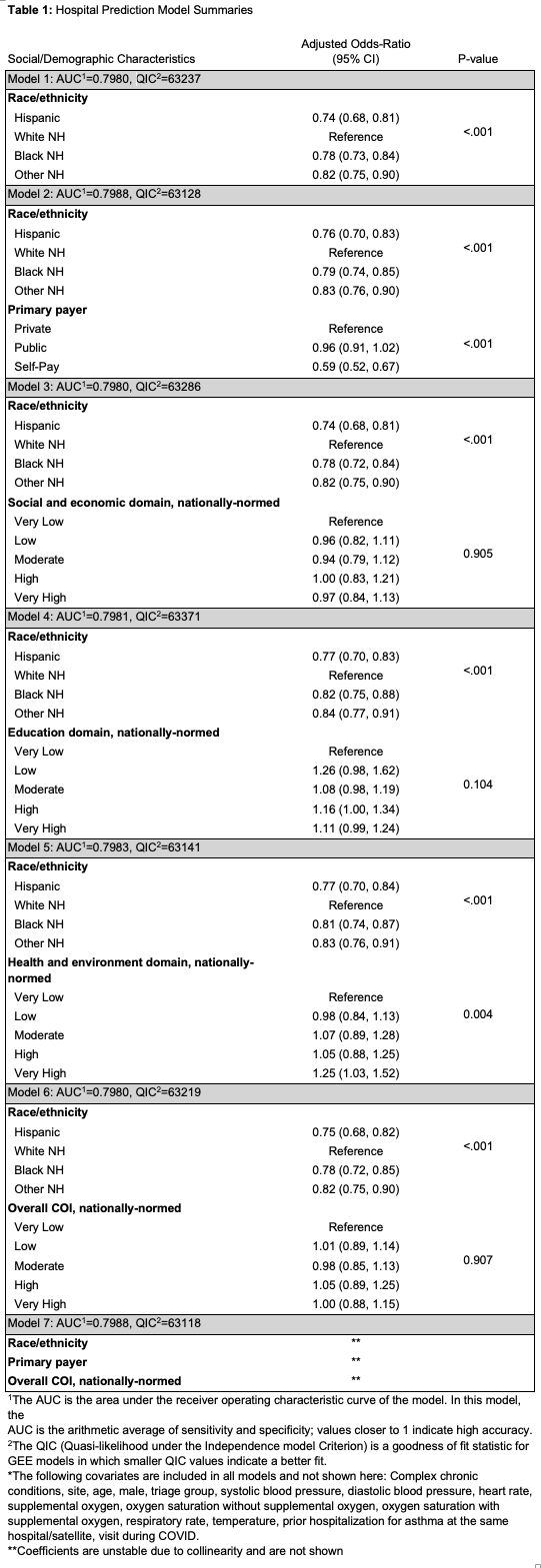
We included 65,855 visits with complete data from January 2017 to December 2020, of whom 26,271 (39.9%) were hospitalized. Hospitalization by overall COI and COI domain is presented in Figure 1. The AUC of the severity-only model was 0.7969. Results of comparative models that include race/ethnicity, payer, overall COI, and individual domains of the COI are presented in Table 1. The maximal AUC of models that included SDoH was 0.7988.
Conclusion(s):
The addition of SDoH to a model that included only severity did not increase the model's predictive accuracy for hospitalization in children with asthma in a large multicenter cohort. The measures we analyzed do not represent all measures of severity or of SDoH, such as chronic asthma control or household income. Additional and more granular information representing severity and SDoH may be needed to quantify the contribution of SDoH to disparities in asthma care in the ED.
.png)