Hospital Medicine: Clinical
Hospital Medicine 7
777 - Post-discharge Thromboprophylaxis Practice Patterns in MIS-C and COVID-19 Pneumonia in Pediatrics: A Survey of US-based Pediatric Hospitalists and Hematologists
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 777
Publication Number: 777.416
Publication Number: 777.416
Harita Katragadda, Children's Health, Dallas, TX, United States; Ayesha Zia, UT Southwestern Medical Center, Dallas, TX, United States
.jpg)
Harita Katragadda, MD (she/her/hers)
Fellow
UT Southwestern/Children's Health
Dallas, Texas, United States
Presenting Author(s)
Background: COVID-19 pneumonia and Multisystem Inflammatory Syndrome in Children (MIS-C) result in prothrombotic states which can persist post-discharge. The International Society of Thrombosis and Haemostasis published COVID-19/MISC-C anticoagulation pediatric guidelines in August 2020, recommending 30 days of post-discharge thromboprophylaxis (PDT) for elevated D-dimer and venous thromboembolism (VTE) risk factors whereas adult guidelines suggest against PDT. We hypothesized that practice variation exists nationally regarding PDT. We surveyed pediatric hospitalists and hematologists about VTE risk assessment and PDT in COVID-19 pneumonia and MIS-C.
Objective: Identify practice variations in pediatric institutions in the US regarding VTE risk assessment and PDT in pediatric patients with COVID-19 pneumonia and MIS-C.
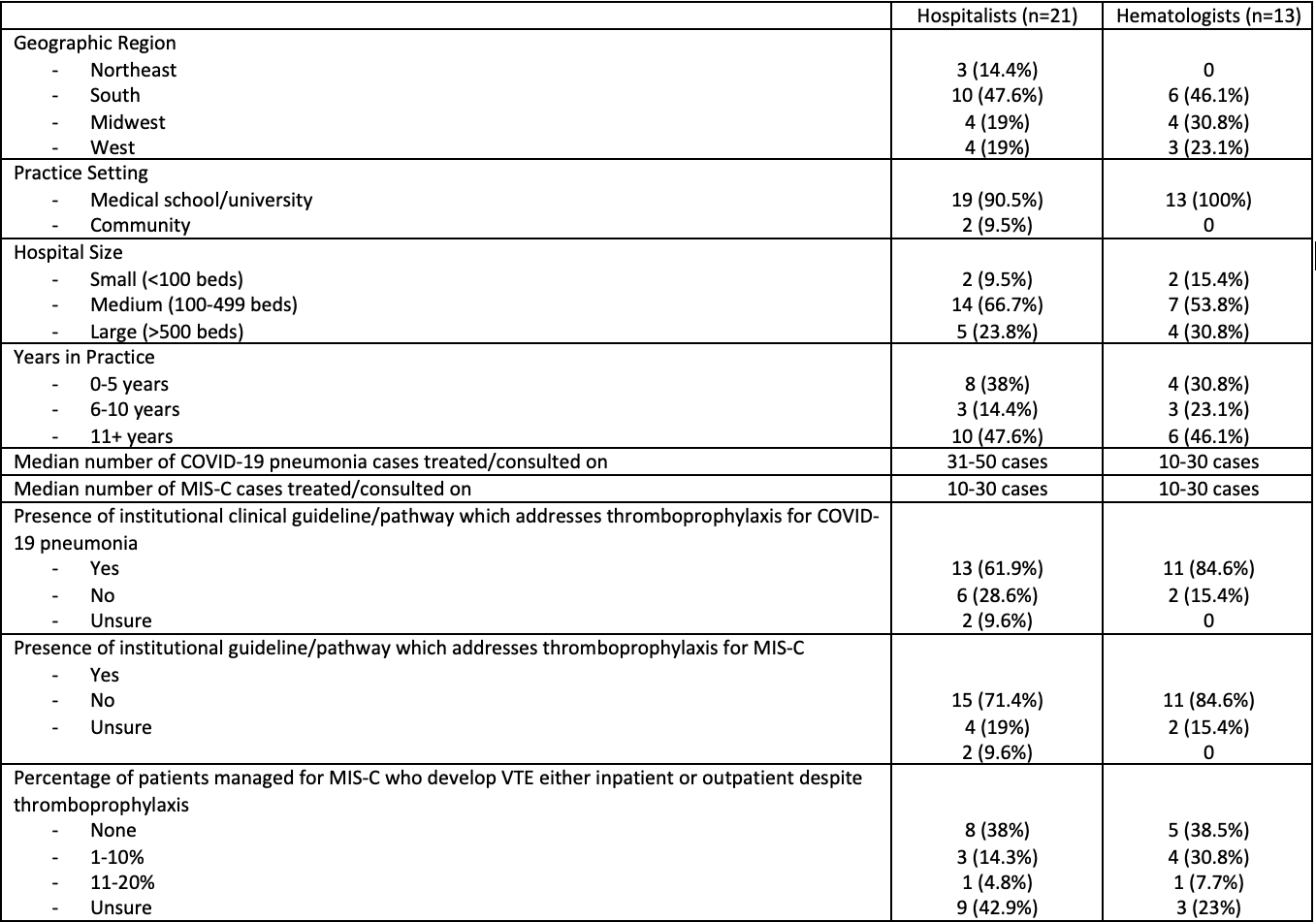
Design/Methods: We used purposive sampling to anonymously survey pediatric hospitalists and hematologists from 25 pediatric hospitals across the US between March 16, 2022, and August 16, 2022. Elements included participant characteristics, approach to risk assessment of hospital acquired VTE, PDT practices, and future research priorities. We summarized key findings and compared results between hospitalists and hematologists.
Results: The response rate of completed surveys was 60.7% (34/56), and we received at least one response from 89% (25/28) of the institutions surveyed. 57% of hospitalists and 69% of hematologists thought that all patients with MIS-C require VTE risk assessment versus 38% of hospitalists and 38.5% of hematologists for COVID-19 pneumonia. Both groups agreed on the top 4 risk factors for VTE in this population. Pediatric hospitalists did not include the presence of central venous catheters, and hematologists did not include thrombophilia in their top 5 VTE risk factors. 33% (95% CI: 15%, 55%) of hospitalists and 25% (95% CI: 7%, 52%) of hematologists reported never prescribing PDT in MIS-C, whereas 22% (95% CI: 8%, 42%) of hospitalists and 25% (95% CI: 7%, 52%) of hematologists for COVID-19 pneumonia. No trends were noted about decisions to prescribe PDT, duration, or follow-up.
Conclusion(s): We report heterogeneity in VTE risk assessment and PDT practices in COVID-19 pneumonia/MIS-C. A quarter to a third of patients with COVID-19 and MIS-C have never been prescribed PDT, irrespective of its severity. Pediatric patients with COVID-19 pneumonia and MIS-C might be exposed to unnecessary anticoagulation with unclear benefits or inadvertently not being anticoagulated when indicated. PDT in this setting requires future research.
.png)
.png)
