Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 5: Surfactant and NIV 2
674 - Optimizing Endotracheal Tube Length Management for Preterm Infants
Publication Number: 674.443
Barry Huang, Bachelor of Science
Medical Student
Creighton University School of Medicine
Omaha, Nebraska, United States
Presenting Author(s)
Background:
Endotracheal intubation is commonly required to assist breathing in preterm neonates with respiratory difficulties. Determining an ideal endotracheal tube (ETT) length must balance reducing airway resistance by decreasing the tube length and, if cut too short, the risk of the patient requiring re-intubation with a longer tube. Additionally, repetitive airway manipulation during re-intubation or tube repositioning positively correlates with airway edema which may influence extubation success rates.
Objective: To infer the optimal length to cut the ETT during initial intubation by assessing the difference between initial ETT depth and depth at extubation. We also sought to evaluate associations between the frequency of airway manipulation and successful extubation.
Design/Methods: This was a retrospective single-center cohort study of infants born at ≤ 32 0/7 weeks of gestation at a single center between August 2012 and December 2021. Infants were excluded if the record was unavailable or incomplete, if they were never intubated or intubated for < 24hr, or if they had an airway or oral malformation. ETT position was normalized to the depth at initial intubation. Subjects were stratified by gestational age (< 28wks vs 28-32wks). Extubation success was defined as remaining extubated for >72hr. We performed multivariable logistic regression to assess associations between the number of ETT adjustments and extubation success, adjusting for potential confounders.
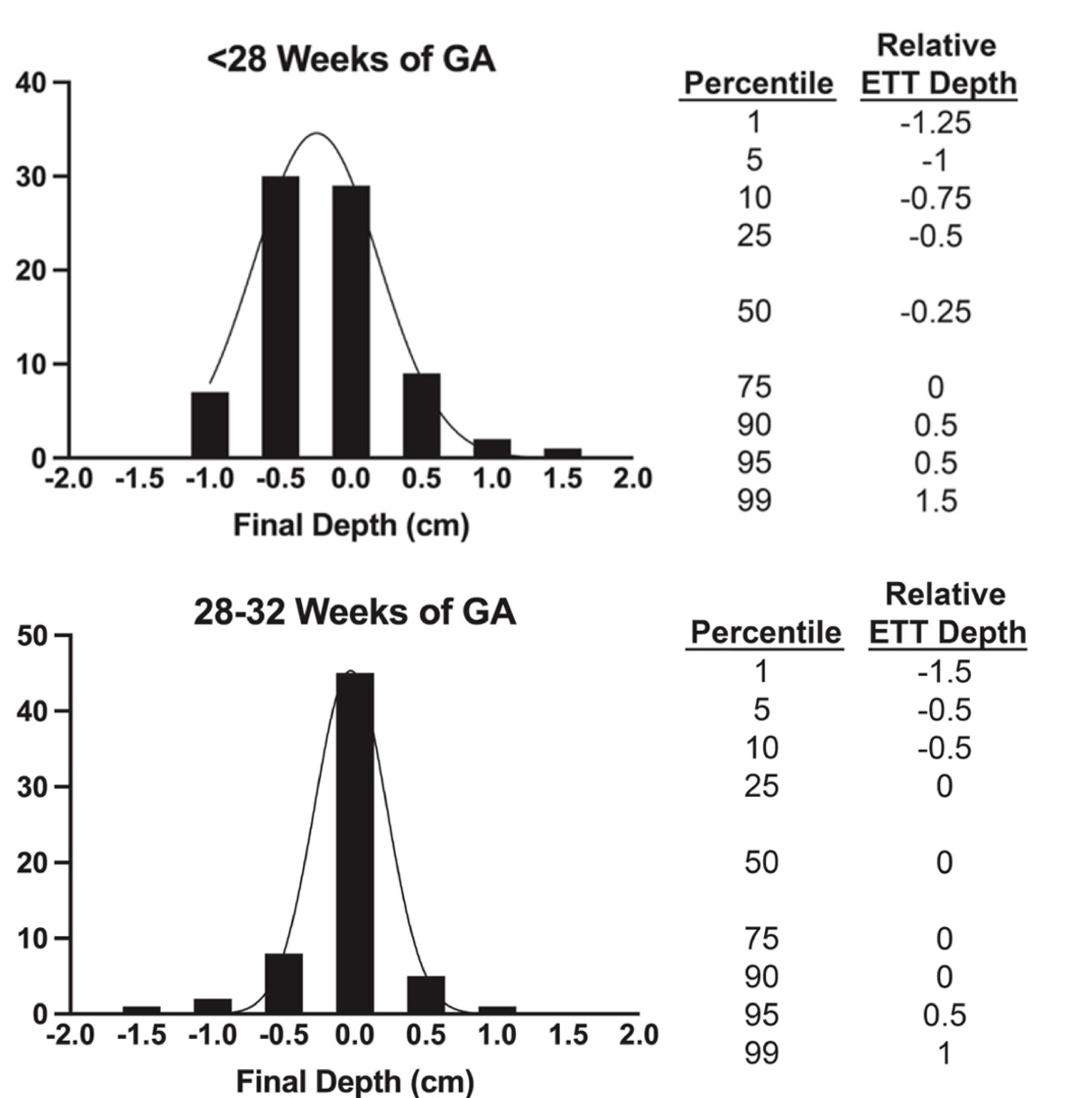
Results: The 95th percentile for both gestational age groups was a relative depth of 0.5 cm, though the 99th percentile differed between the groups (Fig.1). Demographic data compared between initial extubation success or failure revealed significant differences in birth weight and type of delivery in univariate analyses. Multivariable logistic regression analysis demonstrated a significant association between extubation success and duration of primary intubation (OR 1.11, p=0.025) and birth weight (OR=1.00, p=0.035) but not the number of ETT adjustments (OR 1.14, p=0.588), surfactant administration (OR=5.18, p=0.203), or low-dose dexamethasone administration (OR=0.12, p=0.092).
Conclusion(s): This study suggests that trimming the ETT to 1-1.5 cm (plus length needed to secure ETT to face), depending on gestational age, would minimize the risk of requiring re-intubation due to the patient outgrowing the ETT length (in at least 99% of patients) and may optimize the resistance within the ETT. These data also suggest little evidence to support the concern that adjusting the endotracheal tube inside the airway leads to increased rates of extubation failure.