Hospital Medicine: Clinical
Hospital Medicine 3
486 - Descriptive Analysis of a Pediatric Sepsis Alerting System
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 486
Publication Number: 486.221
Publication Number: 486.221
William H. Stafford, University of Tennessee Health Science Center College of Medicine, Memphis, TN, United States; Jerry D. Hagler, University of Tennessee Health Science Center College of Medicine, Cordova, TN, United States; Kathleen Cao, Emory University School of Medicine, Atlanta, GA, United States; Nico N. West, University of Tennessee Health Science Center College of Medicine, Memphis, TN, United States; Bindiya Bagga, UTHSC, Memphis, TN, United States; Samir Shah, UTHSC / Le Bonheur Children's Hospital, Memphis, TN, United States

William H. Stafford, MD, MS (he/him/his)
Pediatrics Resident
University of Tennessee Health Science Center College of Medicine
Memphis, Tennessee, United States
Presenting Author(s)
Background: Patients admitted to pediatric wards with Severe Sepsis (SS) face challenges due to variations in age-based vital signs and lab values. Delayed diagnosis, therapy and escalation of care increase morbidity and mortality. We instituted a novel Electronic Health Record (EHR) integrated Pediatric SS screening tool for children at our institution for real-time identification of Pediatric SS based on the International Consensus Conference on Pediatric Sepsis that was revised to improve alert predictability. Residents, previously educated on recognition/treatment of SS, receive alerts via smartphone. No literature exists describing impact of an electronic alert system for identification of patients with Pediatric SS among pediatric ward units.
Objective: Provide a descriptive analysis of patients admitted to the pediatric ward who triggered an electronic SS alert.
Design/Methods: Records identified by the electronic SS alert screening tool were retrospectively studied through an IRB approved process. Patients aged 1-17 years admitted to pediatric ward who triggered a SS alert were included. ICU and ED patients were excluded. Clinical and laboratory information within 24hrs of the SS alert were reviewed. Primary outcomes included descriptive analysis of the cohort: demographics, comorbidities, microbiology data, antibiotic appropriateness and goal-directed therapy measures. Secondary outcomes included need for ICU transfer and identification of patients with true sepsis.
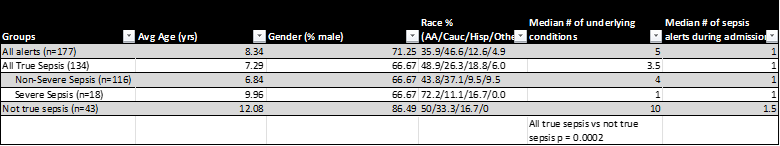
Results: SS alerts (n=177) between March and November 2022 were studied. Of these,134 (75.7%) alerts met true sepsis criteria (2/4 SIRS plus infection). Blood culture was obtained in 40% of patients following SS alert; 5 were positive. Viral testing positivity varied between groups. All patients with true sepsis (100%) were on appropriate antibiotic treatment per institutional stewardship guidelines. Patients with SS had a higher peak CRP than patients without SS (p=0.02). Fluid bolus was given in 33.5% of patients with true sepsis and 55.56% with severe sepsis. Alerts led to ICU transfer in 11.8% of cases. Patients triggering false sepsis alerts had more co-morbidities (p=0.0002) and longer median length of stay (p=0.003).
Conclusion(s): Consistent timely identification of patients with SS admitted to the pediatric ward is feasible by implementing an electronic alert system guiding goal-directed therapy and escalation of care. Resident education likely contributed to appropriate antibiotic use, fluid bolus administration, and diagnostic testing. CRP was a corroborative marker for identifying severe sepsis.
.png)
.png)
