Infectious Diseases
Infectious Diseases 4
422 - Factors Determining Antibiotic Prescriptions for Pediatric Pneumonia in the Emergency Department
Publication Number: 422.418

Maheswari Ekambaram, MBBS (she/her/hers)
Fellow
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background:
Evidence-based guidelines recommend amoxicillin as first-line therapy for community-acquired pneumonia (CAP) in children. Still, recent studies have demonstrated that macrolides and broad-spectrum antibiotics are commonly prescribed. Guideline-discordant antibiotic prescriptions increase the risk of adverse events and contribute to antimicrobial resistance. Predictors of antibiotic choice for CAP in the emergency department (ED) setting are incompletely understood.
Objective:
To identify factors associated with antibiotic prescribing for pediatric CAP among patients discharged from the emergency department.
Design/Methods:
We performed a retrospective cohort study of children 3 months to 18 years discharged from the ED between 2016-2021 with a diagnosis of CAP. Eleven community EDs and a children’s hospital ED from a single healthcare system was included. Patients prescribed amoxicillin, macrolide, or broad-spectrum antibiotics (amoxicillin-clavulanate, 3rd generation cephalosporins, clindamycin, doxycycline, and fluoroquinolone) for CAP were included. We excluded children with medical complexity, severe or complicated pneumonia, and the receipt of multiple antibiotics. We identified predictors of antibiotic choice for CAP using univariate and multivariate logistic regression.
Results:
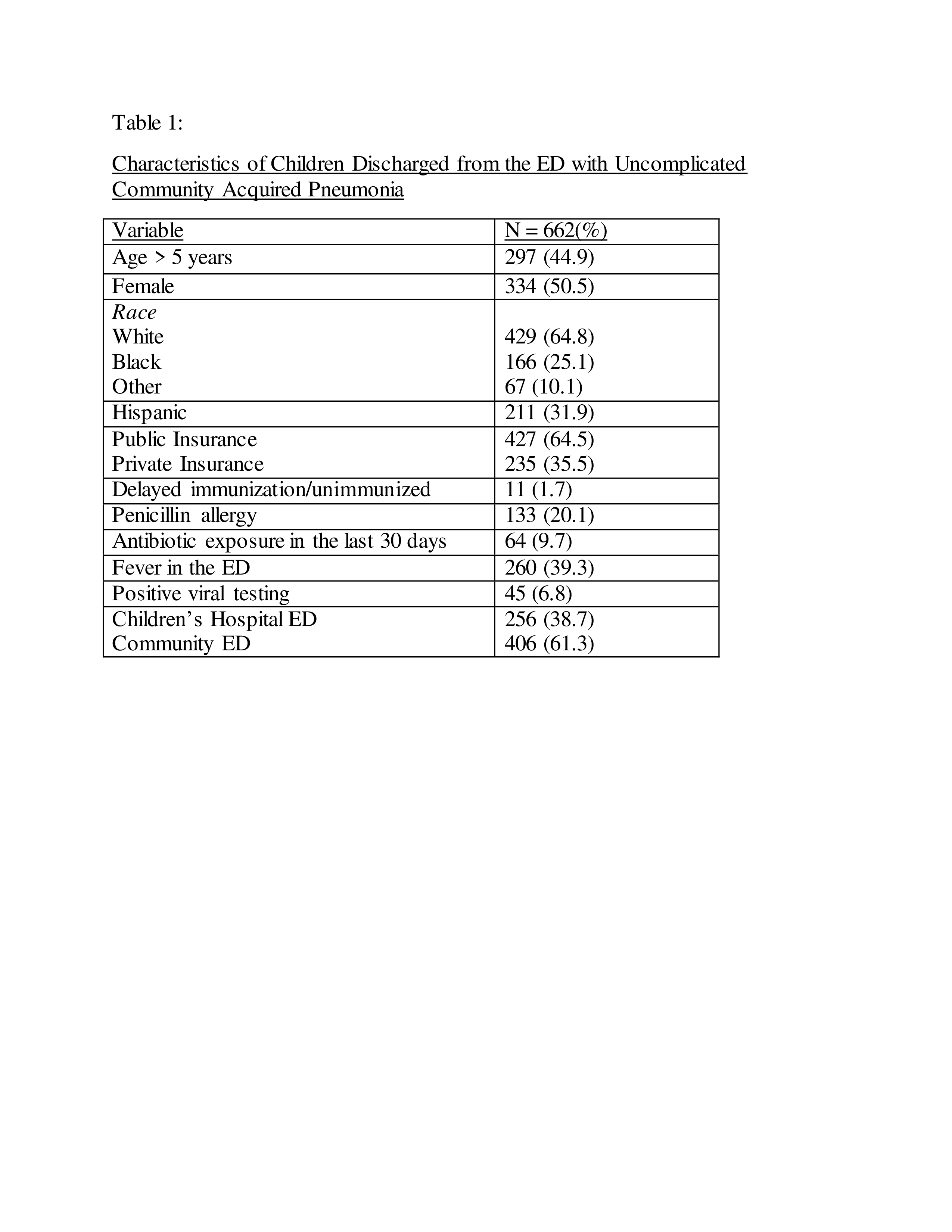
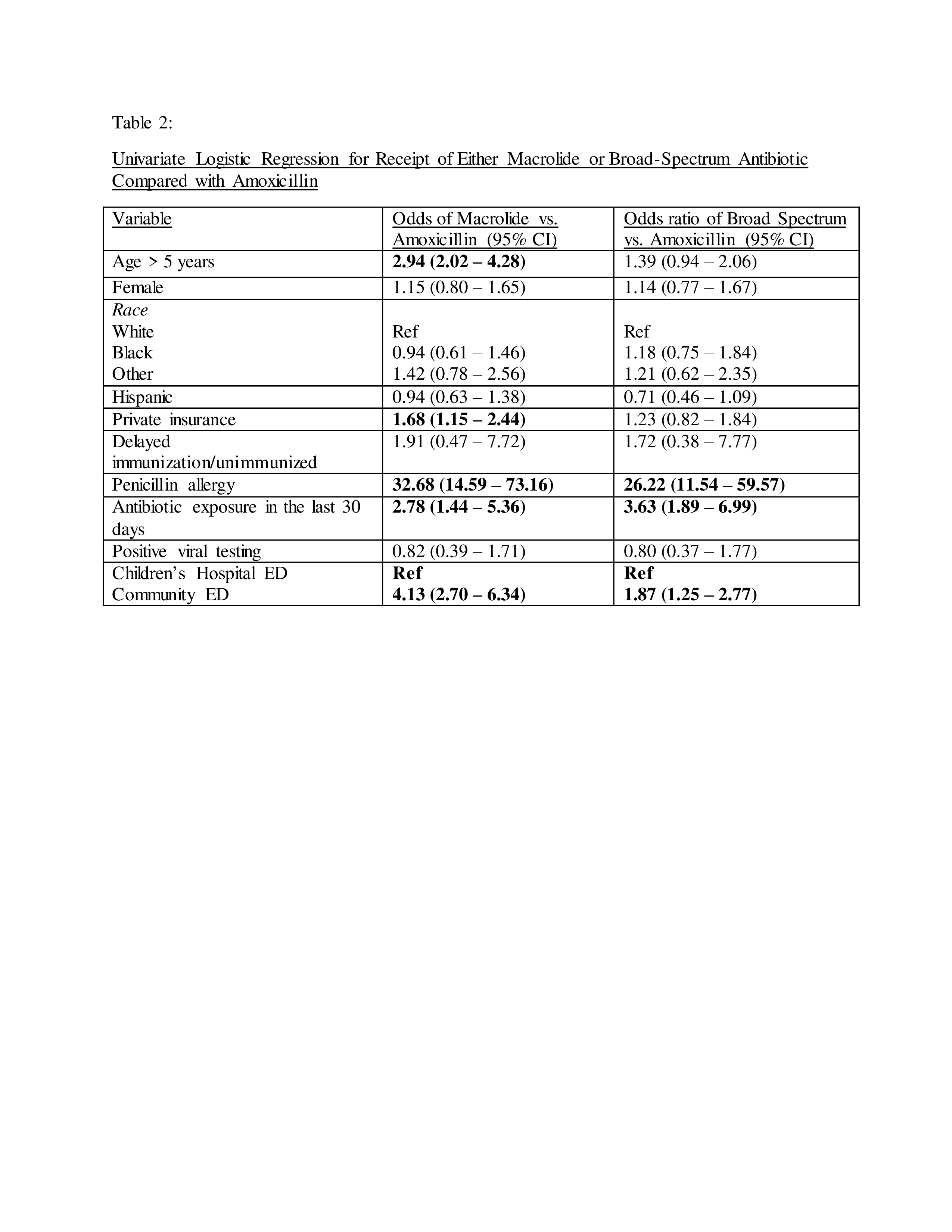
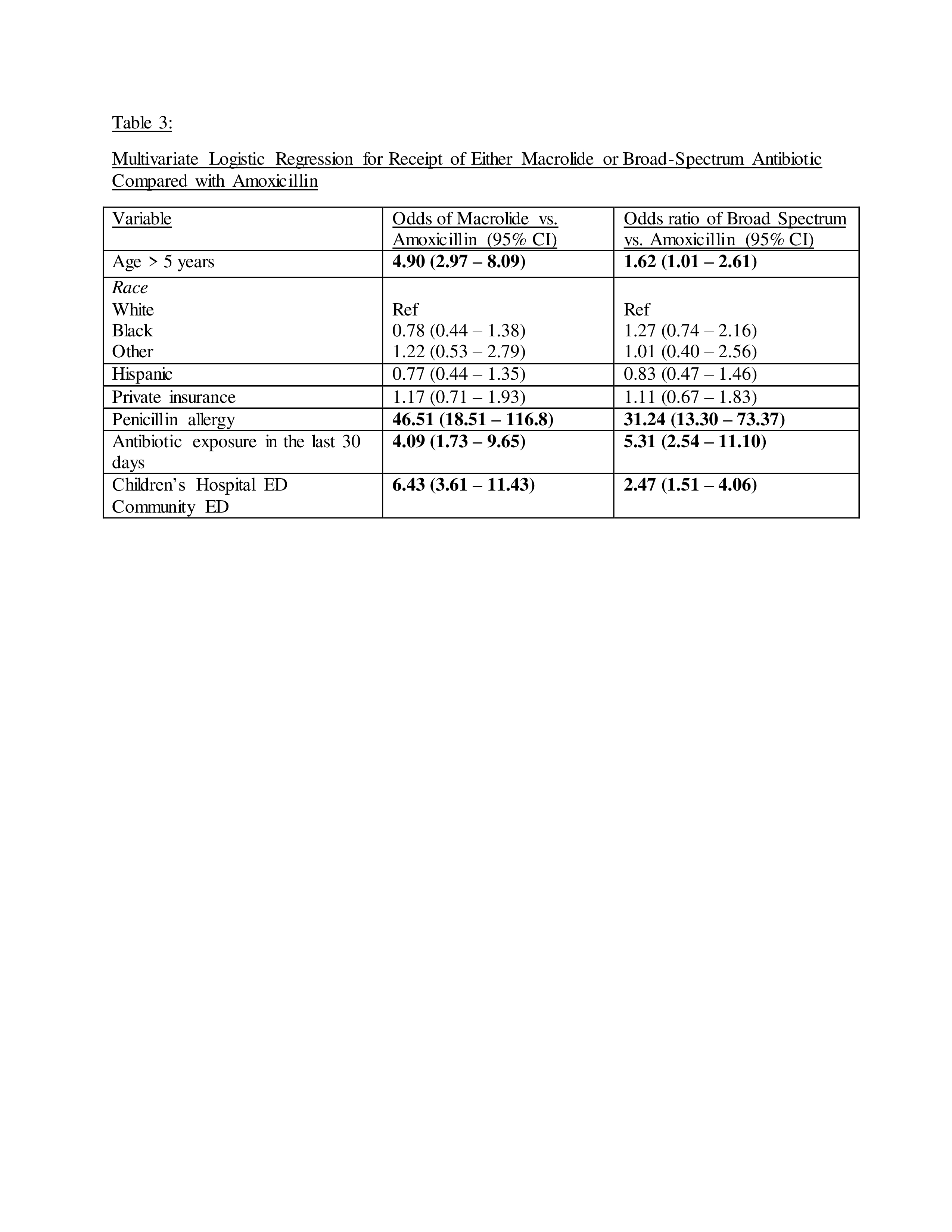
A total of 662 children were included. The majority were under five years of age (55%), white (65%), had public insurance (61%), and were cared for in a community ED (61%) (Table 1). Amoxicillin was prescribed in 51% of children, macrolide in 27%, and broad-spectrum in 22%. In univariate analysis, age over 5 years and private insurance were associated with increased macrolide prescriptions compared with amoxicillin (Table 2). In multivariate regression, age > 5 years, penicillin allergy, antibiotic exposure in the last 30 days, and care in a community ED were associated with increased macrolide and broad-spectrum antibiotic use compared to amoxicillin (Table 3).
Conclusion(s):
Despite national guidelines recommending amoxicillin as the first-line CAP antibiotic, almost half received macrolide or broad-spectrum antibiotics. The antibiotic choice for CAP in the ED was influenced by clinical factors (patient’s age, prior antibiotic exposure, antibiotic allergy) as well as care location. Understanding factors associated with antibiotic choice will help inform tailored antimicrobial stewardship interventions to reduce inappropriate antibiotic use.