Emergency Medicine: All Areas
Emergency Medicine 14
383 - Opportunities and Outcomes of Trainee-Performed Emergent Tracheal Intubations in a Pediatric Emergency Department
Publication Number: 383.405

Douglas A. Potts, Jr., MD (he/him/his)
Fellow
Nationwide Children's Hospital
PICKERINGTON, Ohio, United States
Presenting Author(s)
Background:
Tracheal intubation (TI) is a vital procedure in pediatric resuscitation. Emergency medicine (EM) residents are dependent on limited time in the pediatric emergency department (PED) for pediatric TI opportunities. In our academic pediatric center, pediatric emergency medicine (PEM) fellows or EM residents often perform the first attempt at TI. Subsequent attempts, when needed, can refine technique through immediate corrective adjustments. First-pass success (FPS) in emergent pediatric TI has been reported as 60-75%, but data surrounding second attempt opportunities and success is not typically reported.
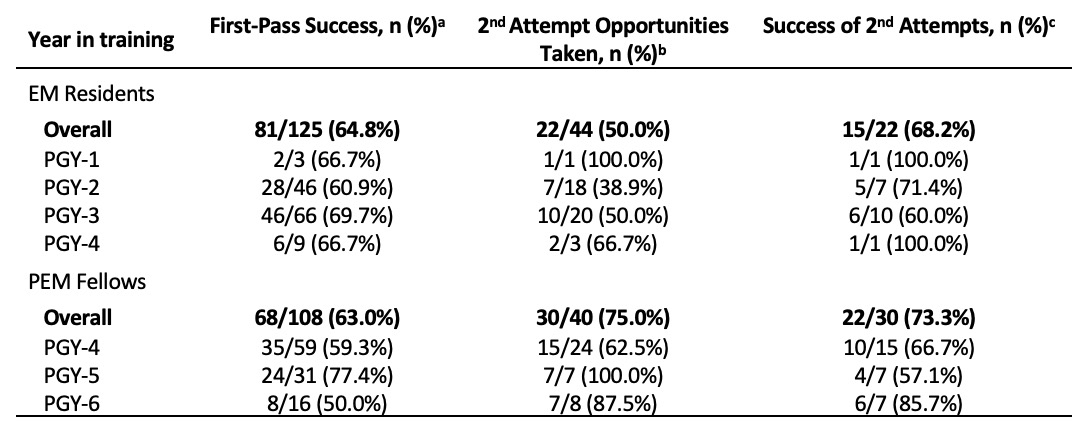
Objective: We reviewed our institution’s trainee TI opportunities. We hypothesized PEM fellows would have higher FPS compared with EM residents, and EM residents would have fewer opportunities to re-attempt a failed intubation.
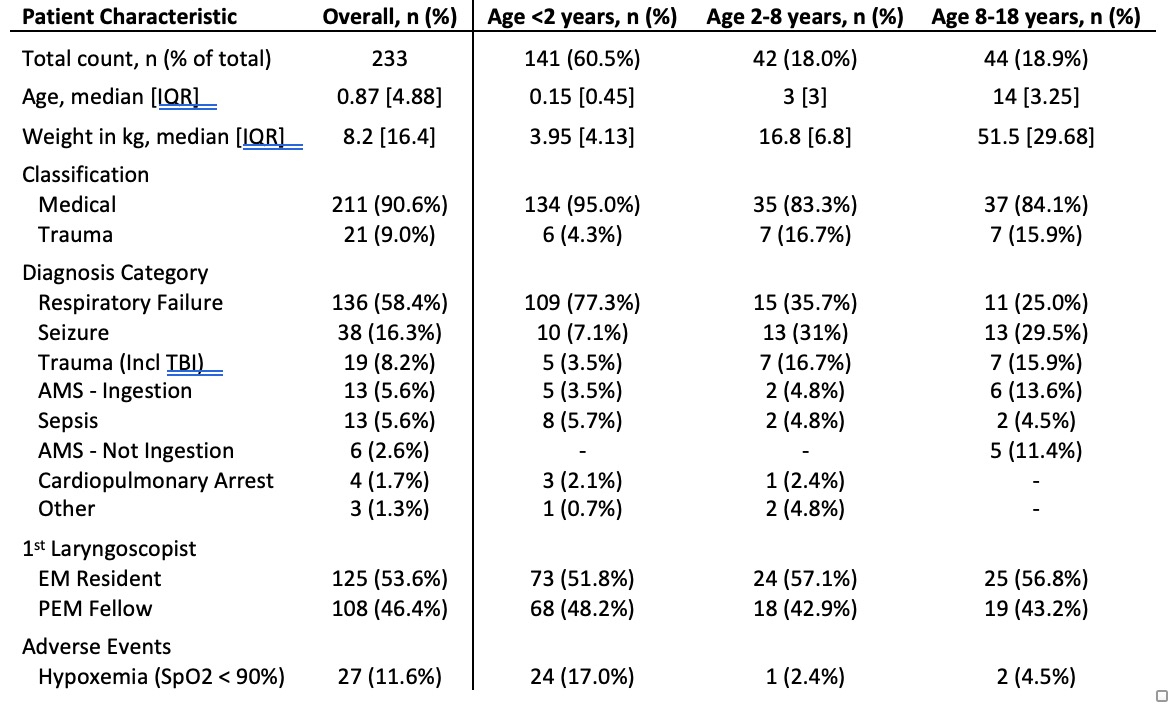
Design/Methods: A retrospective single-center review was performed of a large, academic pediatric emergency department to evaluate trainee-performed tracheal intubations from April 2018 to December 2019. This included a review of the center’s intubation database collected via a combination of video and chart review. Trainee data was added via additional chart and department record review. Outcome measures included first attempt success, opportunity to perform a second attempt, second attempt success and adverse events.
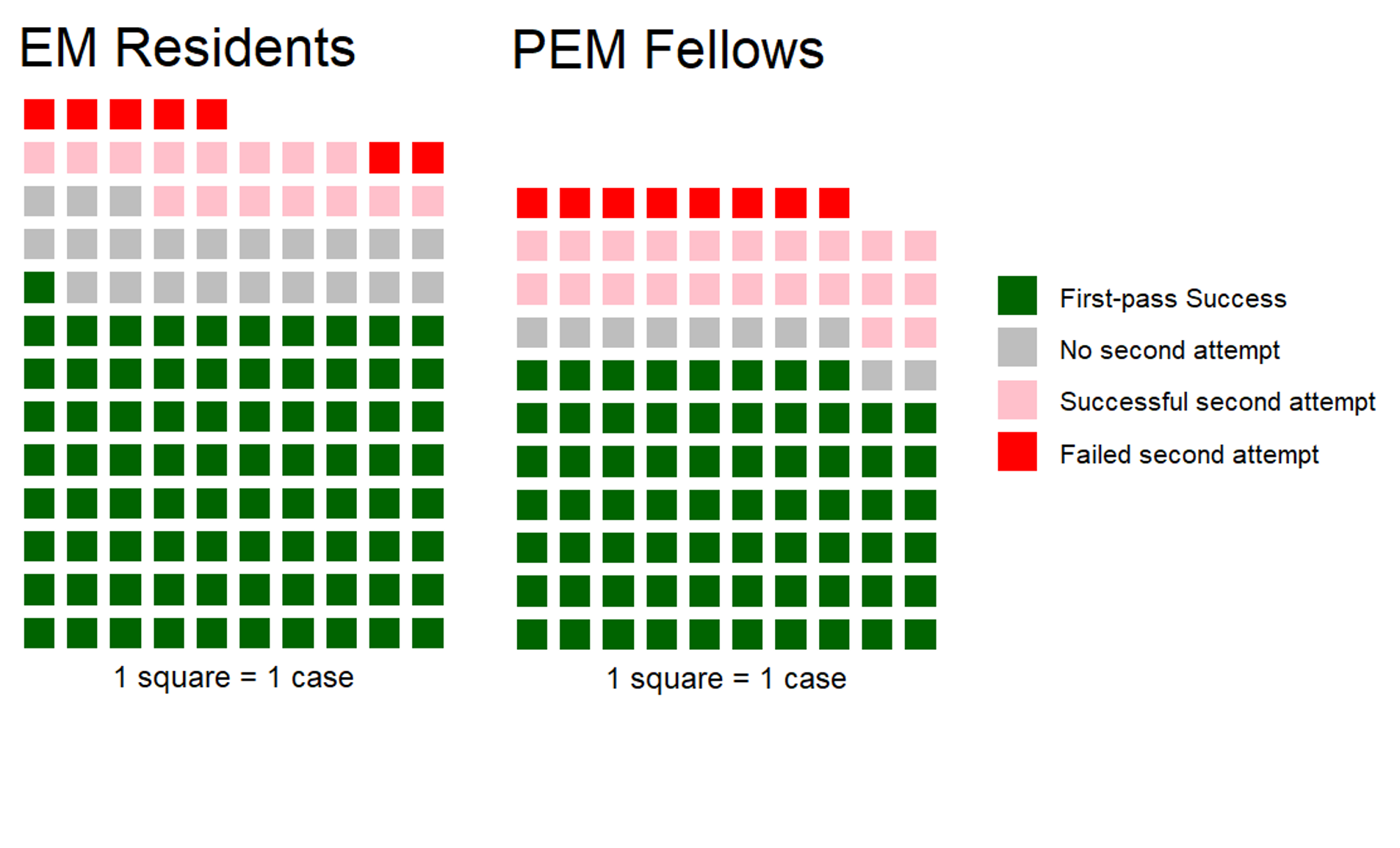
Results: PEM fellows and EM residents performed the first intubation attempt on 233 patients (108, 46.4%; 125, 53.6% respectively) over the study period. FPS for both groups was consistent with previously published data (63.0% and 64.8%). No significant association existed between trainee type and FPS (Odds ratio [OR], 0.92; 95% confidence interval [CI], 0.52-1.64). Overall success rate for both groups was identical (65%). PEM fellows performed a second intubation attempt in 75% of cases in which they had taken the first attempt. EM residents performed a second intubation attempt in 50% of such cases (OR, 2.96; 95% CI, 1.09-8.53). There was no significant difference between laryngoscopist type and second pass success rate (OR, 1.28; 95% CI, 0.32-5.05).
Conclusion(s): In a single center, there was no difference in first or second-attempt success between PEM fellows and EM residents in emergent pediatric TI. However, PEM fellows had nearly three-fold higher odds of being given a second attempt at intubation after a failed attempt compared with EM residents. Given their limited exposure to pediatric TI in training, consideration to allow EM residents subsequent TI attempts could improve proficiency without compromising chances for success.