Neonatal Infectious Diseases/Immunology
Neonatal Infectious Diseases/Immunology 6
460 - Burden of multidrug-resistant neonatal sepsis in secondary level health facilities in India: A prospective multi-centric study On behalf of the Investigators of the District Hospital study
Publication Number: 460.432
- RA
Ramesh Kumar Agarwal, MD DM (he/him/his)
Professor
All India Institute of Medical Sciences, New Delhi
New Delhi, Delhi, India
Presenting Author(s)
Background: The pathogen profile and antimicrobial resistance (AMR) patterns in neonatal sepsis have primarily been reported from tertiary care hospitals. There is a paucity of such data from secondary-level health facilities.
Objective: To evaluate the sepsis burden, pathogens responsible, and antimicrobial resistance patterns among neonates admitted to level-2 units in district hospitals in India.
Design/Methods:
We prospectively followed-up neonates admitted to five level-2 special newborn care units (SNCUs) of the district hospitals between October 2019 and December 2021. A dedicated research team monitored the neonates daily. Blood cultures obtained at the time of suspicion of sepsis were sent to the tertiary sites’ microbiology laboratories for processing. The pathogen was identified and tested for antibiotic susceptibility testing (AST) pattern as per CLSI guidelines. Identification and AST were further confirmed at the nodal center through MALDI-TOF and VITEK, respectively.
Results:
6612 neonates (3972 inborn and 2640 outborn) were enrolled at the five SNCUs. The mean (SD) gestation and birth weight were 37.1 (2.9) weeks and 2536 (690) g, respectively. About half of enrolled neonates were suspected of sepsis. Of all enrolled neonates, 215 (3.3%) and 2090 (31.6%) were diagnosed with culture-positive and culture-negative sepsis, respectively. About 70% of neonates with culture-positive sepsis presented before 72 hours of age. The case-fatality rates (CFR) among neonates with culture-positive and culture-negative sepsis were 36% and 4%, respectively. The CFR was almost 2-fold in outborn (43%) compared to inborn neonates (25%) with culture-positive sepsis.
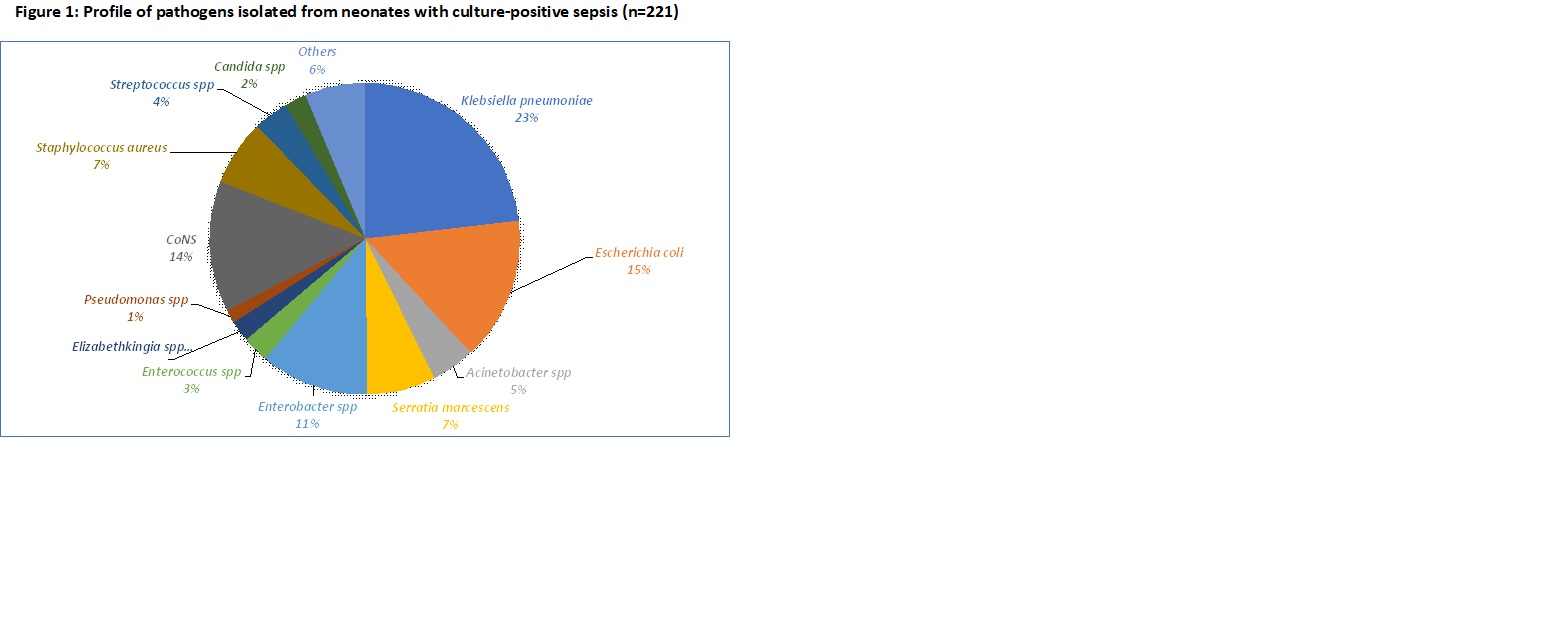
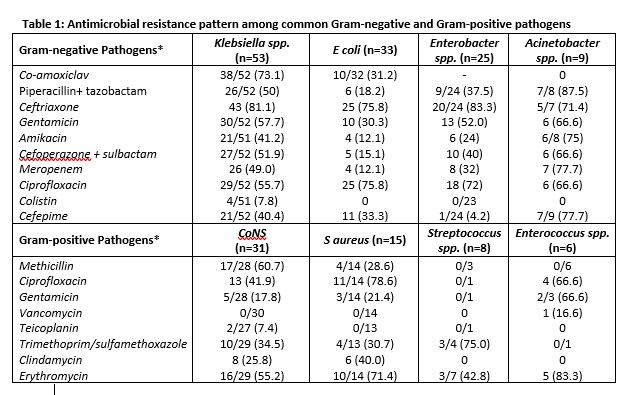
Gram-negative pathogens accounted for about 70% of culture-positive sepsis. Klebsiella spp. (23%), E coli (15%), and Enterobacter spp. (11%) were the most common Gram-negative organisms. CoNS (14%), S aureus (7%), and Streptococcus spp. (4%) were the commonest Gram-positive pathogens (Figure 1). About 50-80% of isolates of Klebsiella spp., Enterobacter spp., and Acinetobacter spp. were resistant to third-generation cephalosporins and gentamicin, while around half of Klebsiella spp. and Acinetobacter spp. were resistant to meropenem (Table 1). About 60% of CoNS were methicillin-resistant.
Conclusion(s):
The high degree of antimicrobial resistance (AMR) to third-generation cephalosporins and carbapenems observed in secondary-level health facilities suggests that the threat of AMR is not confined to tertiary care hospitals alone. It underscores the need to implement antimicrobial stewardship programs in district-level hospitals.