Back
Background: Pediatric end of life (EOL) events are high-acuity and low occurrence, however no specific EOL training is required for pediatric providers. Distress is high among caregivers as they care for children at EOL, and implications for quality of care are significant for dying children and their surviving family members. Increased competence in EOL care is a crucial step toward improved care and decreased clinician death distress. Existing pediatric EOL care skills (PECS) workshops for pediatric fellow trainees have proved efficacious and feasible. As optimal EOL care is provided by an interprofessional team, we expanded the workshop scope to include pediatric residents, pediatric advanced practice nursing students, and clinical social work students.
Objective: To evaluate the feasibility and effectiveness of adapting an existing EOL skills workshop to interprofessional trainees and expanding the curriculum to encompass interprofessional education (IPE).
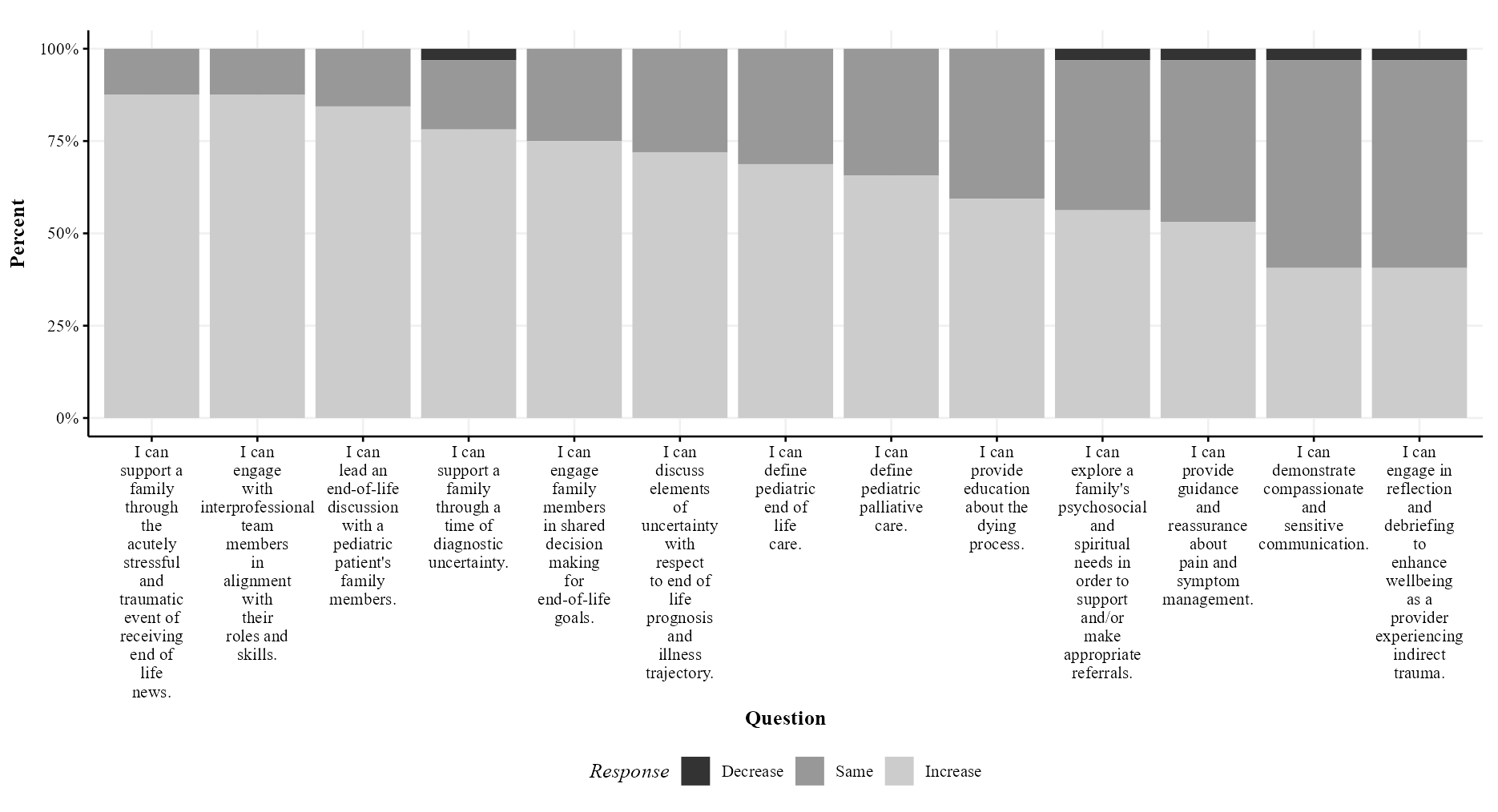
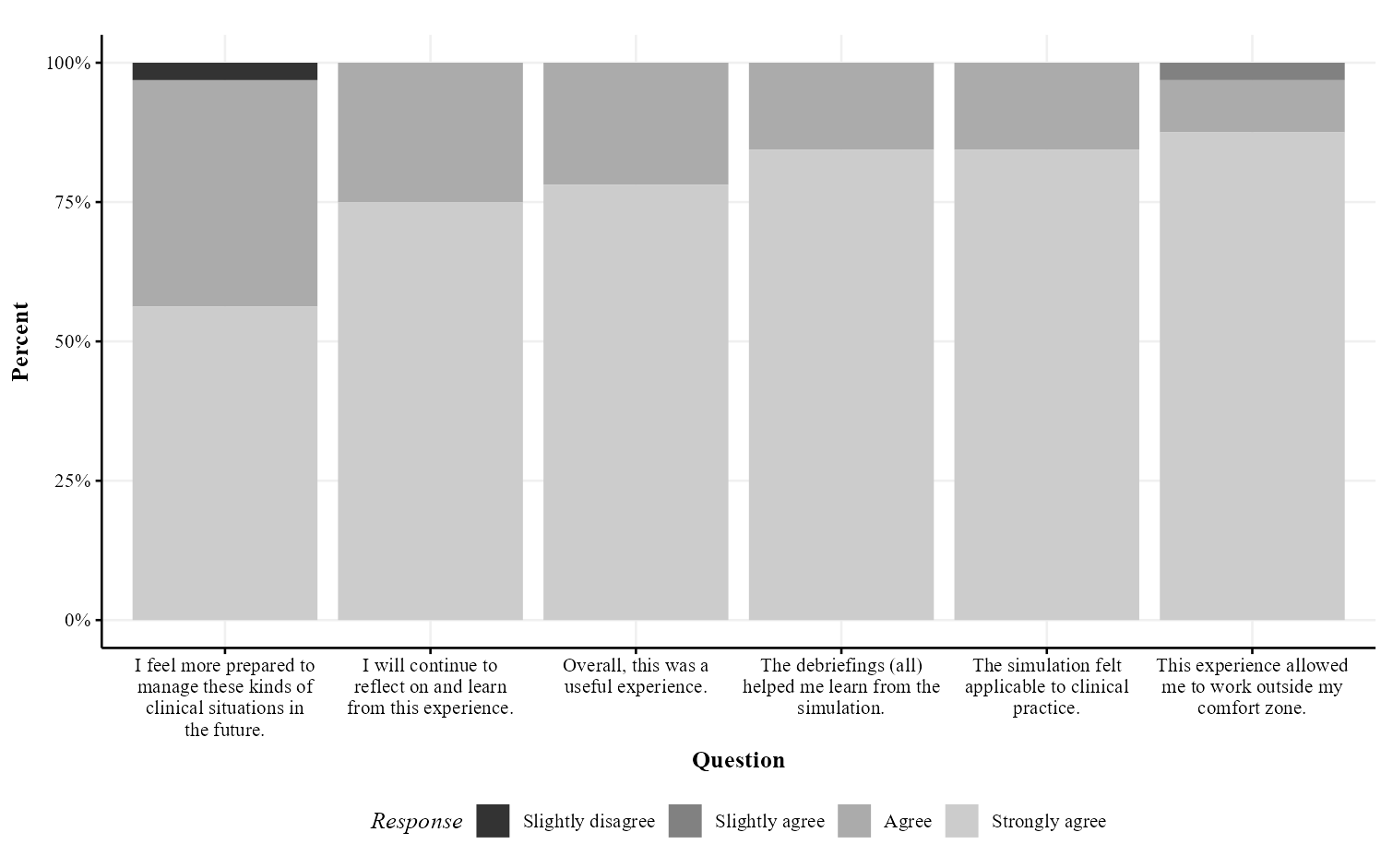
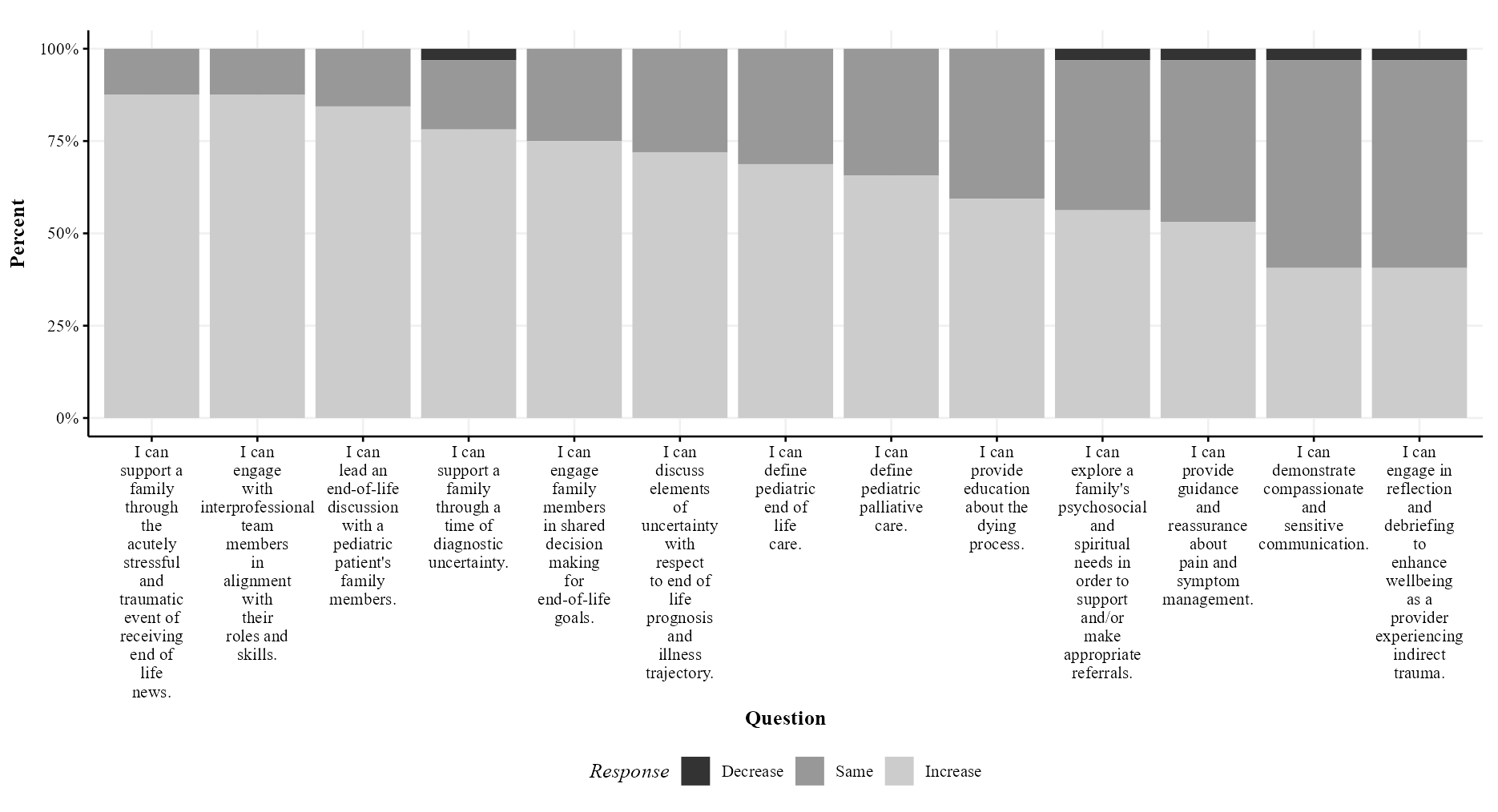
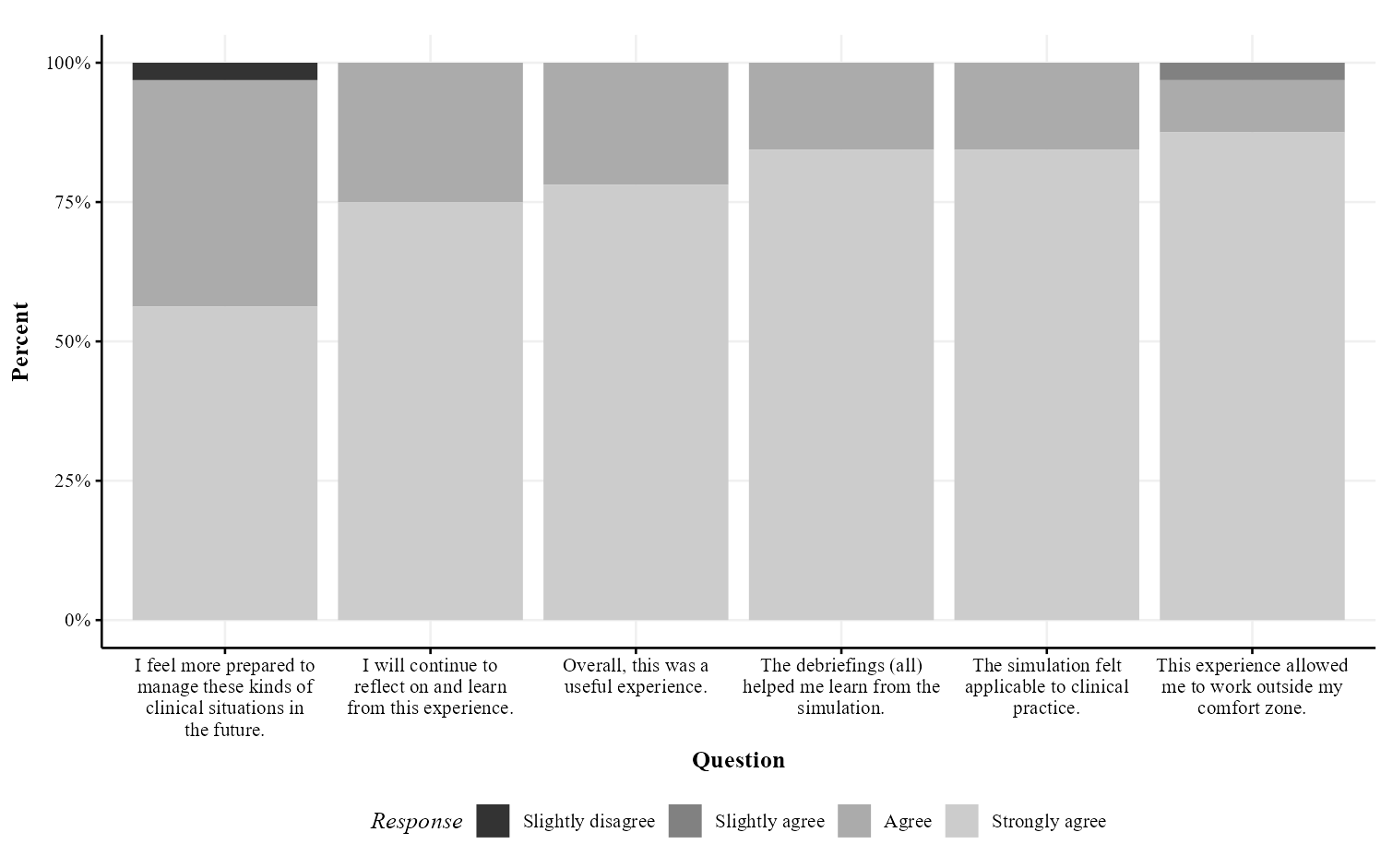
Design/Methods: We conducted 3 pilot interprofessional PECS workshops in 2022. Following each four-hour workshop, participants completed a self-assessment survey of the change in their skill level before vs after the workshop. Questions targeted key knowledge elements and competencies in providing EOL care including the ability to engage in an interprofessional team. Responses on knowledge questions before vs after the workshop were rescored to indicate decreased knowledge, stability, or increased knowledge. All survey responses were summarized with count (%) and visualized with stacked bar plots.
Results: For the 3 pilot workshops, we were successful in scheduling across 3 professional training programs and in recruiting and engaging 33 interprofessional trainees and 27 interprofessional facilitators (roles: physician, nurse, spiritual health, bereaved parent, and social work). All participants completed surveys. In all surveyed domains, nearly all trainees either remained stable or improved in their self-assessment of skill level before vs after the workshop (Figure 1). All trainees found this workshop to be a valuable learning experience across multiple objectives (Figure 2).
Conclusion(s): The expansion of PECS workshops to include interprofessional trainees and IPE goals is feasible, effective, and provides a critical learning opportunity in a safe environment. Future steps will focus on optimizing the workshop content for IPE and longer-term follow-up relating workshop learnings to ongoing clinical practice.
Palliative Care
Palliative Care
428 - Pediatric End of Life Care Skills: An Interprofessional Workshop to Build Competence and Resilience
Friday, April 28, 2023
5:15 PM – 7:15 PM ET
Poster Number: 428
Publication Number: 428.147
Publication Number: 428.147
Miriam C. Shapiro, University of Minnesota Medical School, Minneapolis, MN, United States; Rebecca L. Freese, University of Minnesota, Minneapolis, MN, United States; Susan O'Conner-Von, University of Minnesota, School of Nursing, St Paul, MN, United States; Stacy S. Remke, University of Minnesota, Minneapolis, MN, United States; Anne Woll, University of Minnesota, Minneapolis, MN, United States; Heidi Kamrath, University of Minnesota Medical School, St. Paul, MN, United States; Scheurer M. Johannah, University of Minnesota Medical School, Minneapolis, MN, United States
- MS
Miriam C. Shapiro, MD (she/her/hers)
Assistant Professor, Pediatrics
University of Minnesota Medical School
Minneapolis, Minnesota, United States
Presenting Author(s)
Background: Pediatric end of life (EOL) events are high-acuity and low occurrence, however no specific EOL training is required for pediatric providers. Distress is high among caregivers as they care for children at EOL, and implications for quality of care are significant for dying children and their surviving family members. Increased competence in EOL care is a crucial step toward improved care and decreased clinician death distress. Existing pediatric EOL care skills (PECS) workshops for pediatric fellow trainees have proved efficacious and feasible. As optimal EOL care is provided by an interprofessional team, we expanded the workshop scope to include pediatric residents, pediatric advanced practice nursing students, and clinical social work students.
Objective: To evaluate the feasibility and effectiveness of adapting an existing EOL skills workshop to interprofessional trainees and expanding the curriculum to encompass interprofessional education (IPE).
Design/Methods: We conducted 3 pilot interprofessional PECS workshops in 2022. Following each four-hour workshop, participants completed a self-assessment survey of the change in their skill level before vs after the workshop. Questions targeted key knowledge elements and competencies in providing EOL care including the ability to engage in an interprofessional team. Responses on knowledge questions before vs after the workshop were rescored to indicate decreased knowledge, stability, or increased knowledge. All survey responses were summarized with count (%) and visualized with stacked bar plots.
Results: For the 3 pilot workshops, we were successful in scheduling across 3 professional training programs and in recruiting and engaging 33 interprofessional trainees and 27 interprofessional facilitators (roles: physician, nurse, spiritual health, bereaved parent, and social work). All participants completed surveys. In all surveyed domains, nearly all trainees either remained stable or improved in their self-assessment of skill level before vs after the workshop (Figure 1). All trainees found this workshop to be a valuable learning experience across multiple objectives (Figure 2).
Conclusion(s): The expansion of PECS workshops to include interprofessional trainees and IPE goals is feasible, effective, and provides a critical learning opportunity in a safe environment. Future steps will focus on optimizing the workshop content for IPE and longer-term follow-up relating workshop learnings to ongoing clinical practice.