Back
Background: Infants under 60 days of age with fevers have traditionally undergone extensive workups to rule out serious bacterial infections (SBIs), as prior guidelines often recommend analysis of blood, urine, and cerebrospinal fluid. The American Academy of Pediatrics (AAP) released updated guidelines that use clinical judgment, shared decision-making, and screening inflammatory markers (IMs) to better identify infants with high SBI risk. While both guidelines suggest that neonates under 22 days receive a full sepsis workup, new guidelines suggest foregoing invasive or resource-intensive parts of the workup in well-appearing, full term infants 22 to 60 days old. In this group, clinicians can first obtain IMs before deciding who needs urine cultures, lumbar punctures (LPs), intravenous (IV) antibiotics, and hospital admissions (HAs).
Objective: The primary aim is to validate the new AAP guidelines by applying them to well-appearing, full term infants 22 to 60 days old and assessing accuracy of SBI detection. A secondary aim is to determine if old guidelines suggest overutilization of hospital resources (defined as LP, IV antibiotic use, and HA).
Design/Methods: Infants presenting to our pediatric emergency department (ED) from January 2017 to December 2019 were retrospectively reviewed if they were well-appearing, full term, and 22 to 60 days old with reported fever of 38.0 C or higher. Clinical, laboratory, and demographic data was obtained from the electronic medical record. The incidences of urine cultures, LPs, IV antibiotics and HAs were measured for each patient and compared to recommendations by old and new guidelines. Patient outcomes and discrepancies between the two guidelines were noted.
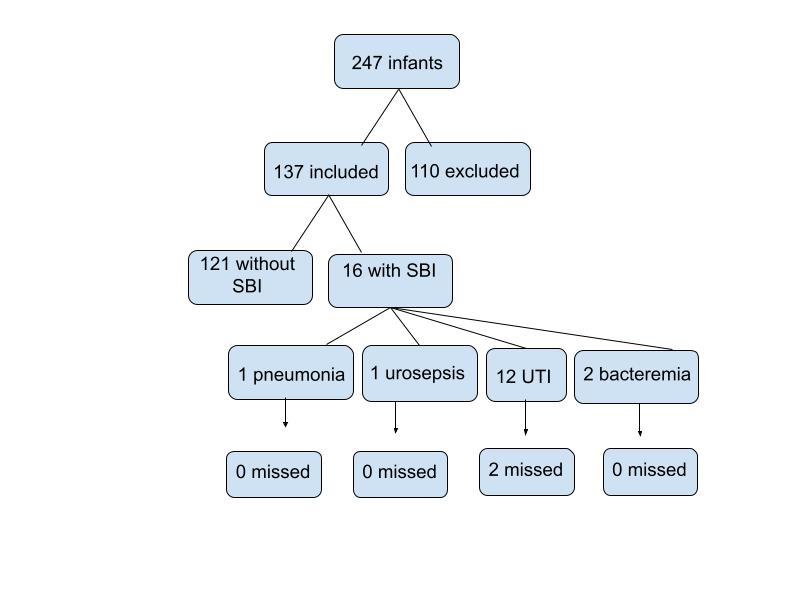
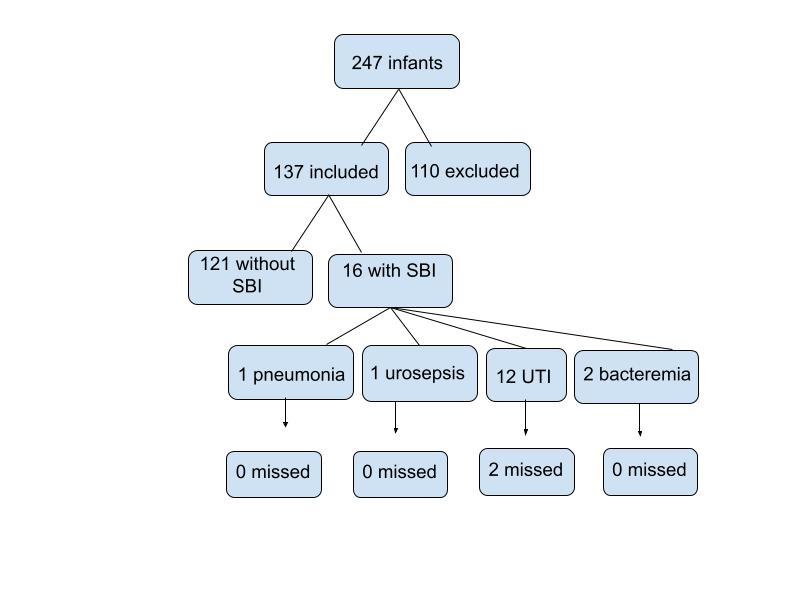
Results: Of the 247 infants reviewed, 137 (55%) met inclusion criteria. 16 infants had SBIs (11.6%). Of those with SBIs, 12 (75%) had urinary tract infections (UTIs). 2 UTIs (16%) would be missed using the new guidelines. Among the 137 infants, the new guidelines recommended 20 less LPs, 19 less IV antibiotics, and 16 less HAs than the old guidelines. No SBIs were missed in cases where less workup was suggested.
Conclusion(s): 2 UTIs were missed under the new guideline’s recommendations, which suggest urine cultures do not need to be sent if a screening urinalysis (UA) is negative. Rarely, urine cultures grow bacteria in the absence of a positive UA. Overall, the new guidelines suggest a decrease in workups for well-appearing, full term infants between 22 to 60 days of age while missing few SBIs. With this, infants may avoid risks of invasive workups, and pediatric departments may conserve more resources.
Emergency Medicine: All Areas
Emergency Medicine 3
58 - A Retrospective Validation of Updated Febrile Infant Guidelines
Friday, April 28, 2023
5:15 PM – 7:15 PM ET
Poster Number: 58
Publication Number: 58.112
Publication Number: 58.112
Kriti Gupta, New York-Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY, United States; Christopher Kelly, NewYork-Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY, United States

Kriti Gupta, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
New York-Presbyterian Brooklyn Methodist Hospital
Brooklyn, New York, United States
Presenting Author(s)
Background: Infants under 60 days of age with fevers have traditionally undergone extensive workups to rule out serious bacterial infections (SBIs), as prior guidelines often recommend analysis of blood, urine, and cerebrospinal fluid. The American Academy of Pediatrics (AAP) released updated guidelines that use clinical judgment, shared decision-making, and screening inflammatory markers (IMs) to better identify infants with high SBI risk. While both guidelines suggest that neonates under 22 days receive a full sepsis workup, new guidelines suggest foregoing invasive or resource-intensive parts of the workup in well-appearing, full term infants 22 to 60 days old. In this group, clinicians can first obtain IMs before deciding who needs urine cultures, lumbar punctures (LPs), intravenous (IV) antibiotics, and hospital admissions (HAs).
Objective: The primary aim is to validate the new AAP guidelines by applying them to well-appearing, full term infants 22 to 60 days old and assessing accuracy of SBI detection. A secondary aim is to determine if old guidelines suggest overutilization of hospital resources (defined as LP, IV antibiotic use, and HA).
Design/Methods: Infants presenting to our pediatric emergency department (ED) from January 2017 to December 2019 were retrospectively reviewed if they were well-appearing, full term, and 22 to 60 days old with reported fever of 38.0 C or higher. Clinical, laboratory, and demographic data was obtained from the electronic medical record. The incidences of urine cultures, LPs, IV antibiotics and HAs were measured for each patient and compared to recommendations by old and new guidelines. Patient outcomes and discrepancies between the two guidelines were noted.
Results: Of the 247 infants reviewed, 137 (55%) met inclusion criteria. 16 infants had SBIs (11.6%). Of those with SBIs, 12 (75%) had urinary tract infections (UTIs). 2 UTIs (16%) would be missed using the new guidelines. Among the 137 infants, the new guidelines recommended 20 less LPs, 19 less IV antibiotics, and 16 less HAs than the old guidelines. No SBIs were missed in cases where less workup was suggested.
Conclusion(s): 2 UTIs were missed under the new guideline’s recommendations, which suggest urine cultures do not need to be sent if a screening urinalysis (UA) is negative. Rarely, urine cultures grow bacteria in the absence of a positive UA. Overall, the new guidelines suggest a decrease in workups for well-appearing, full term infants between 22 to 60 days of age while missing few SBIs. With this, infants may avoid risks of invasive workups, and pediatric departments may conserve more resources.