Palliative Care
Palliative Care
429 - Results of a Pediatric Resident Hospice/Palliative Medicine Curriculum Needs Assessment
Publication Number: 429.147
.jpg)
Ingrid Frydson, MD
Pediatric Resident
Baylor College of Medicine
San Antonio, Texas, United States
Presenting Author(s)
Background:
A recent scoping review revealed that although resident palliative care education has improved, gaps in content, delivery, learner assessment, and evaluation remain. Moreover, published complex care (CC) entrustable professional activities (EPAs) and American Board of Pediatrics content specifications mandate inclusion of goals of care discussions, pain management, critical care, and end-of-life decision-making in pediatric resident training. Our program has an established CC curriculum addressing the care of children with medical complexity (CMC) that does not include a dedicated hospice and palliative medicine (HPM) curriculum.
Objective: We aimed to identify priorities in HPM curriculum design by first conducting a needs assessment within our pediatric residency program.
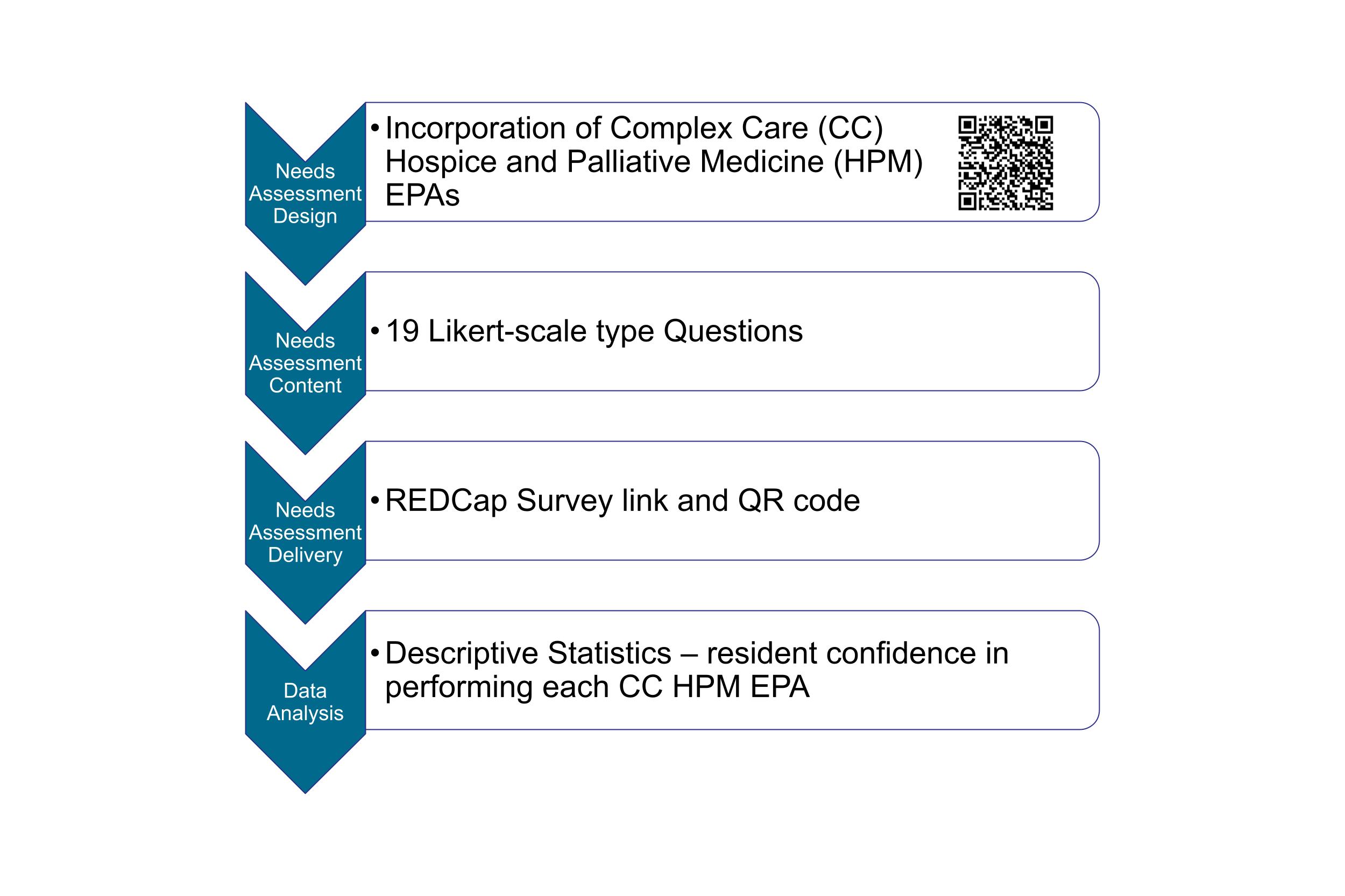
Design/Methods: Using CC EPAs, we designed an HPM curriculum needs assessment. The needs assessment presented 19 Likert-scale type questions, assessing pediatric resident confidence when engaging in activities related to HPM competencies for CMC. We used descriptive statistics to illustrate resident confidence in performing each CC HPM EPA.
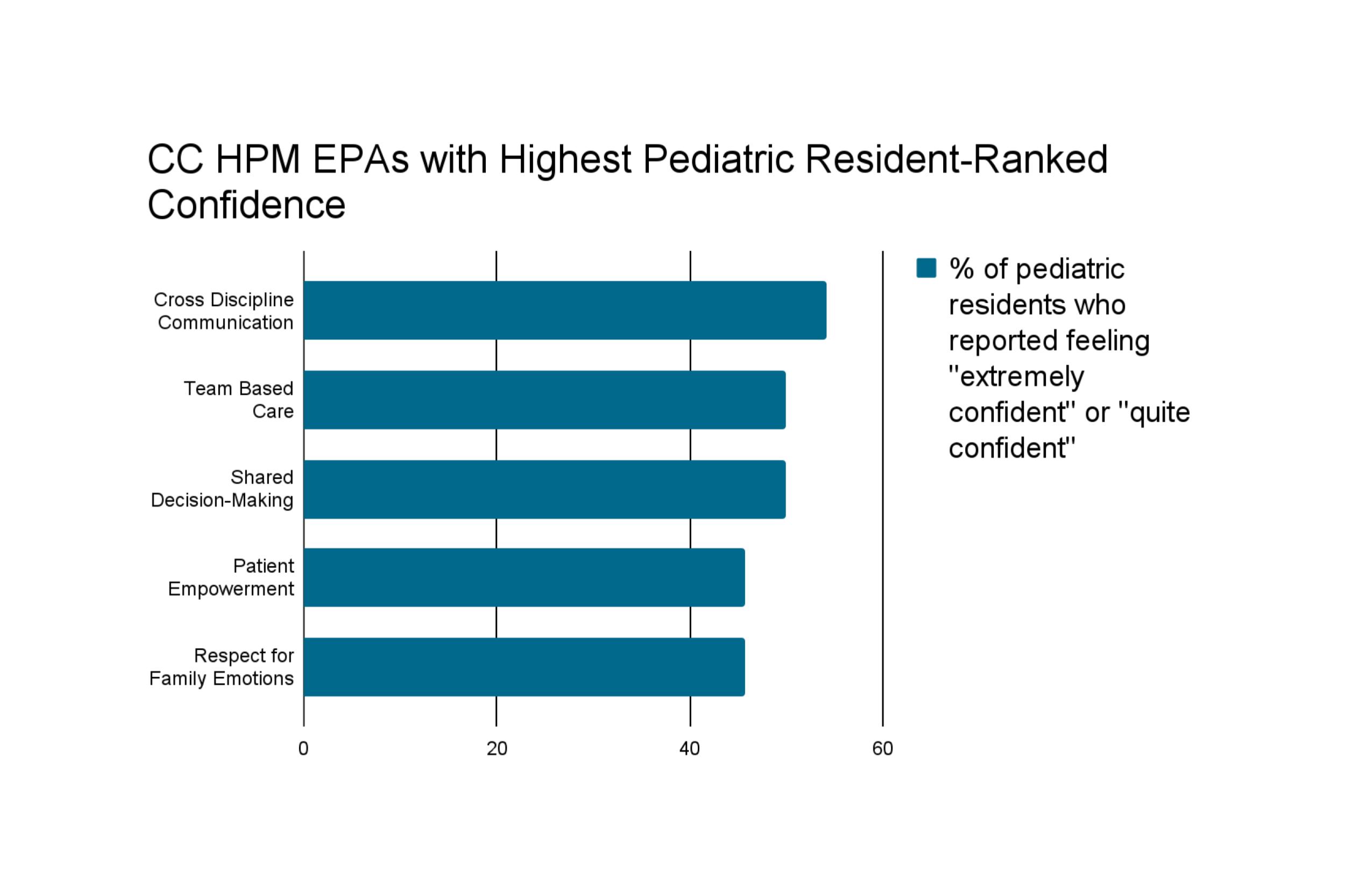
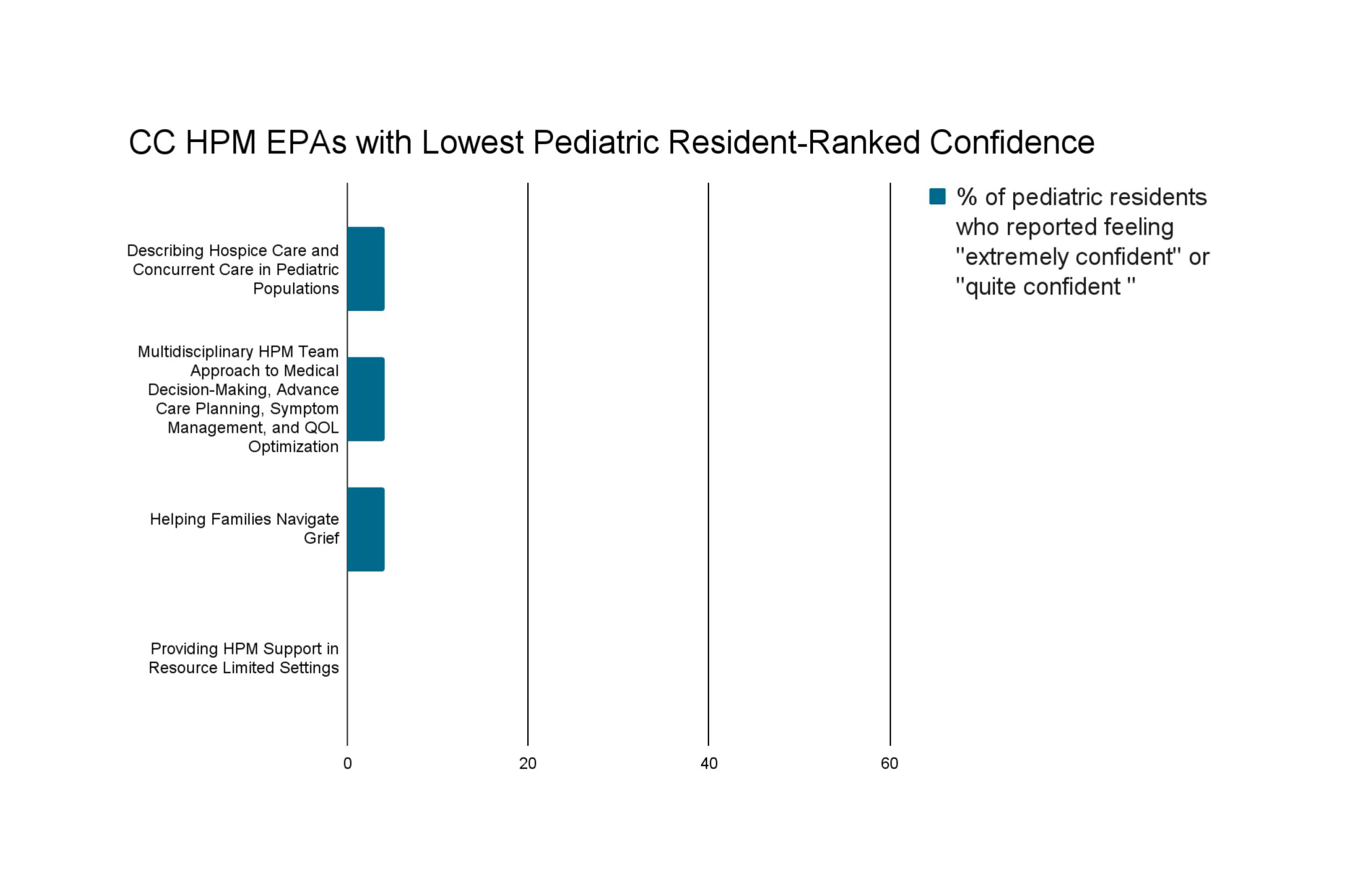
Results: Of 36 residents, 24 (66%) completed the needs assessment. Residents reported feeling “extremely confident” or “quite confident” in cross-discipline communication (54.2%), team-based care (50%), shared decision-making (50%), patient empowerment (45.8%), and respect for family emotions (45.8%), topics delivered via the CC curriculum. On the other hand, few residents reported feeling “extremely confident” or “quite confident” upon self-assessment of confidence in competencies related specifically to HPM: describing hospice care and concurrent care in pediatric populations (4.2%); multidisciplinary HPM team approach to medical decision-making, advance care planning, symptom management, and QOL optimization (4.2%); helping families navigate grief (4.2%); and providing HPM support in resource-limited settings (0%).
Conclusion(s): Our HPM needs assessment demonstrates a gap in pediatric HPM education. Results support an augmentation of the current CC curriculum to include a HPM curriculum that will address these remaining gaps.