Medical Education: Resident
Medical Education 16: Potpourri 1
520 - How Residents Grieve and How We Can Help: Lessons from the Residency Grief Support Team
Monday, May 1, 2023
9:30 AM - 11:30 AM ET
Poster Number: 520
Publication Number: 520.424
Publication Number: 520.424
Hailey Z. Evans, Hassenfeld Children's Hospital at NYU Langone, New York, NY, United States; Rebecca Lois, Hassenfeld Children's Hospital at NYU Langone, New York, NY, United States; Erin Cicalese, New York University Grossman School of Medicine, New York, NY, United States
.jpeg.jpg)
Hailey Zie Evans, MD (she/her/hers)
Chief Resident
Hassenfeld Children's Hospital at NYU Langone
New York, New York, United States
Presenting Author(s)
Background: Physician grief differs from traditional bereavement, as we must set aside emotions in the moment to care for other patients. This delay in processing may be more prominent in first-line providers, such as residents. There is limited data to suggest that protected debriefing sessions for residents, which previously did not exist in our program, are helpful to promote wellness at work and healthy coping strategies.
Objective: The Resident Grief Support Team (RGST) was designed and implemented at the start of the 22-23 academic year (AY). It involves regularly scheduled debriefing and didactic sessions run by a chief resident during protected conference time, and a team of resident volunteers to provide immediate support to colleagues who lose a patient while on call. Our aim is to improve the sense of support and promote development of effective coping skills in our program.
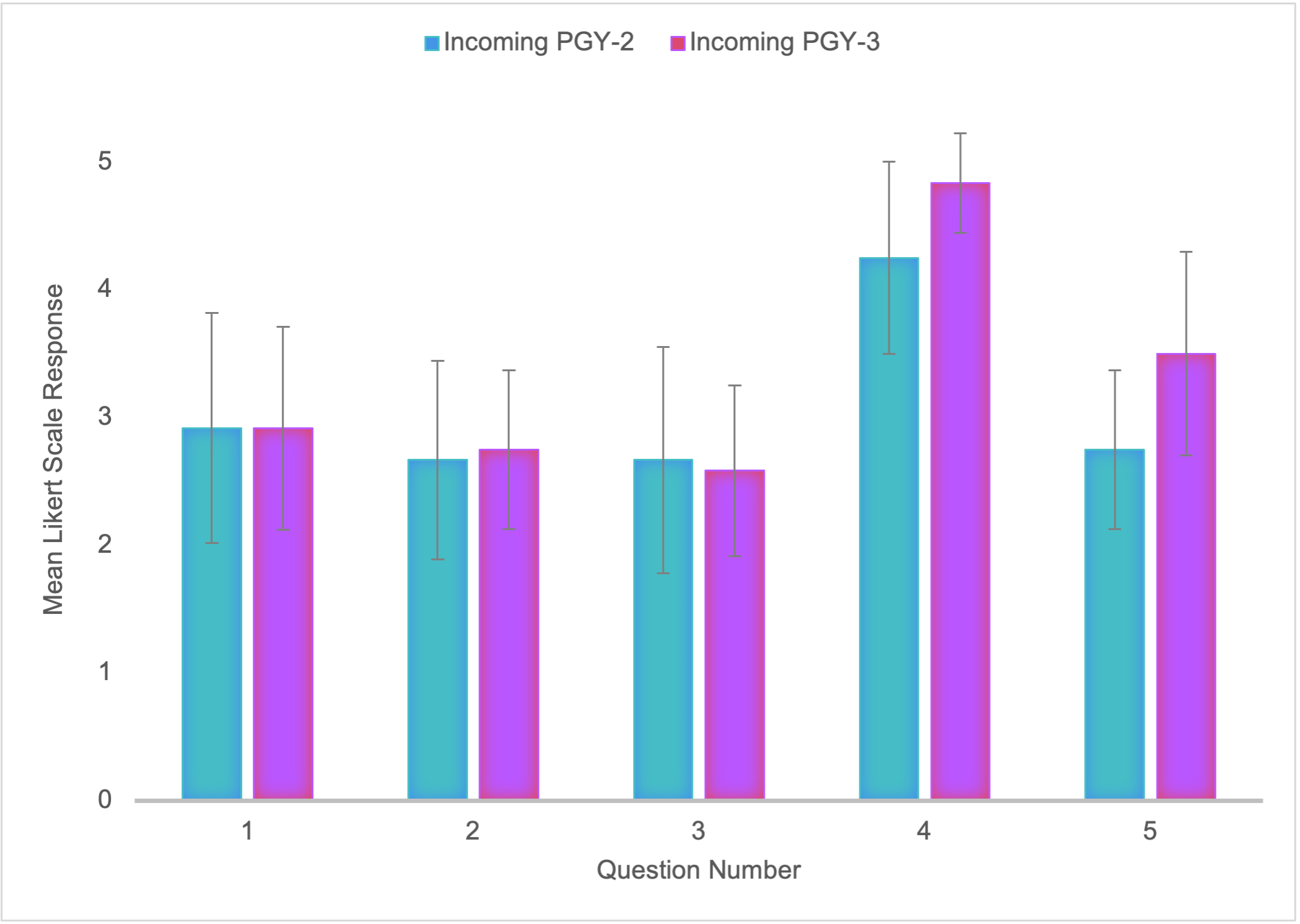
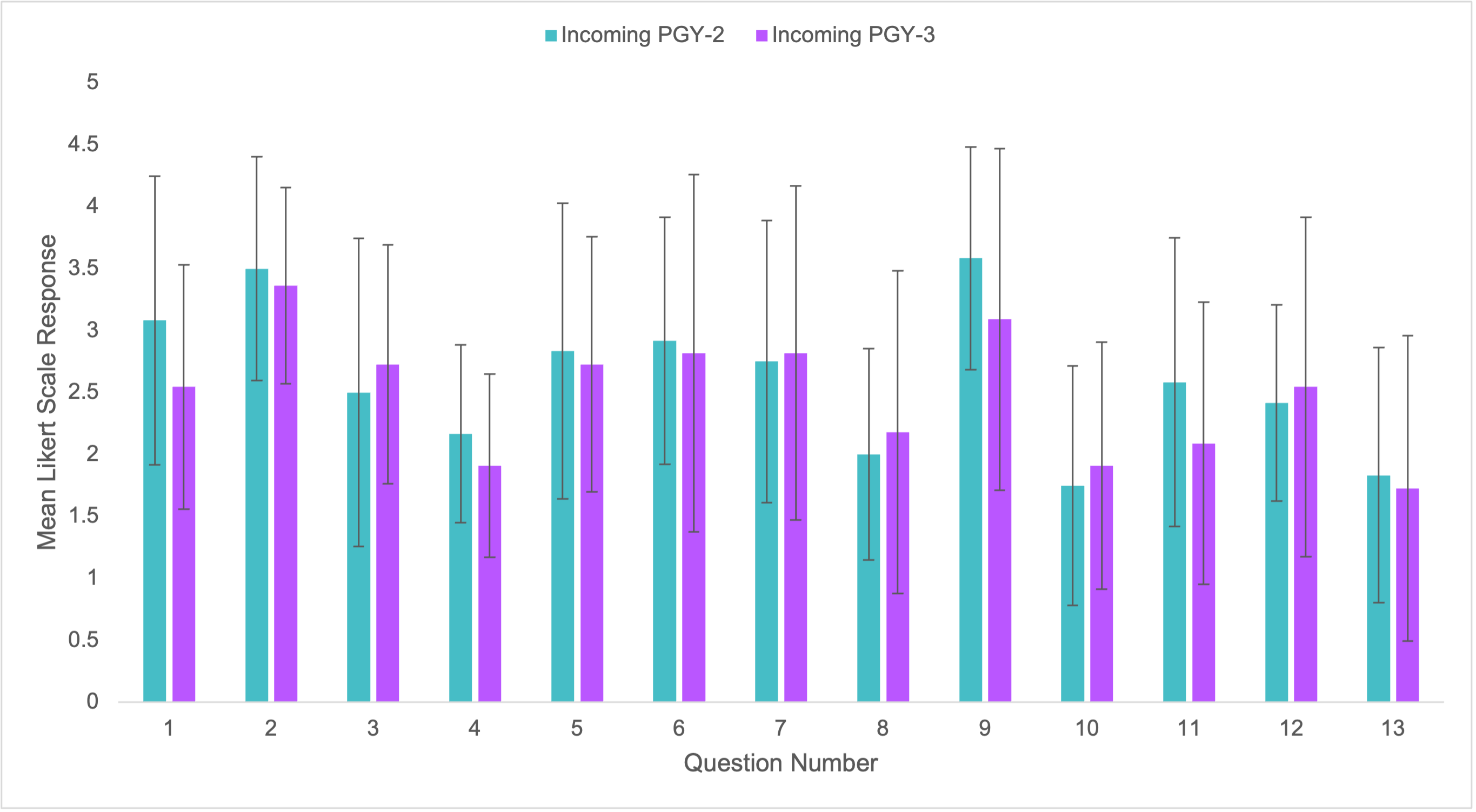
Design/Methods: Anonymous survey data was collected from pediatric residents prior to implementation of RGST and will be collected midway through the AY and at the end of the AY. Data included questions about residents' satisfaction with patient debriefs, comfort speaking with their colleagues about death, and sense of support from the program. Additionally, questions modeled after the Revised Impact of Events Scale (IES-R) assessed level psychological trauma inflicted by difficult cases. All questions were administered using a 1-5 likert scale.
Results: Pre-RGST implementation, residents reported feeling somewhat supported (M=2.9) by their program and somewhat satisfied with the resources provided for resident grief at work (M=2.8) and outside of work (M=2.6). They felt very comfortable speaking with their peers about patient deaths (M=4.5) and less comfortable speaking with their attendings (M=3.1). Regarding psychological trauma (IES-R items), residents more commonly endorsed the following: “when a patient dies or is upsetting me for another reason…” “I have strong waves of feeling about it” (M=3.5), “I push it out of my mind” (M=3.3), “I avoid processing my feelings about it” (M=2.9), and “I have trouble focusing on tasks” (M=2.8). At the time of presentation, all post-intervention data will have been collected and analyzed for any significant differences pre- to post.
Conclusion(s): Our data demonstrate baseline inadequate support for resident grief in our community, as well as evidence of psychological trauma associated with challenging patient cases. Follow up data will be shared at the time of presentation and prove helpful in understanding the impact of a structured grief debrief process.