Emergency Medicine: All Areas
Emergency Medicine 15
399 - The Clinical Impact of Under-Triage in the Pediatric Emergency Department
Publication Number: 399.406

Nichole McCollum, MD (she/her/hers)
PEM Attending, Assistant Professor of Pediatrics and Emergency Medicine
George Washington University School of Medicine and Health Sciences
Washington, District of Columbia, United States
Presenting Author(s)
Background:
Under-triage is the underestimation of acuity or resource needs during the triage process. Because triage occurs at the start of the patient encounter, and sets the stage for the entire clinical visit, under-triage has serious implications for patient care.
Objective: The objective of this study was to measure the clinical impact of under-triage on process measures of care.
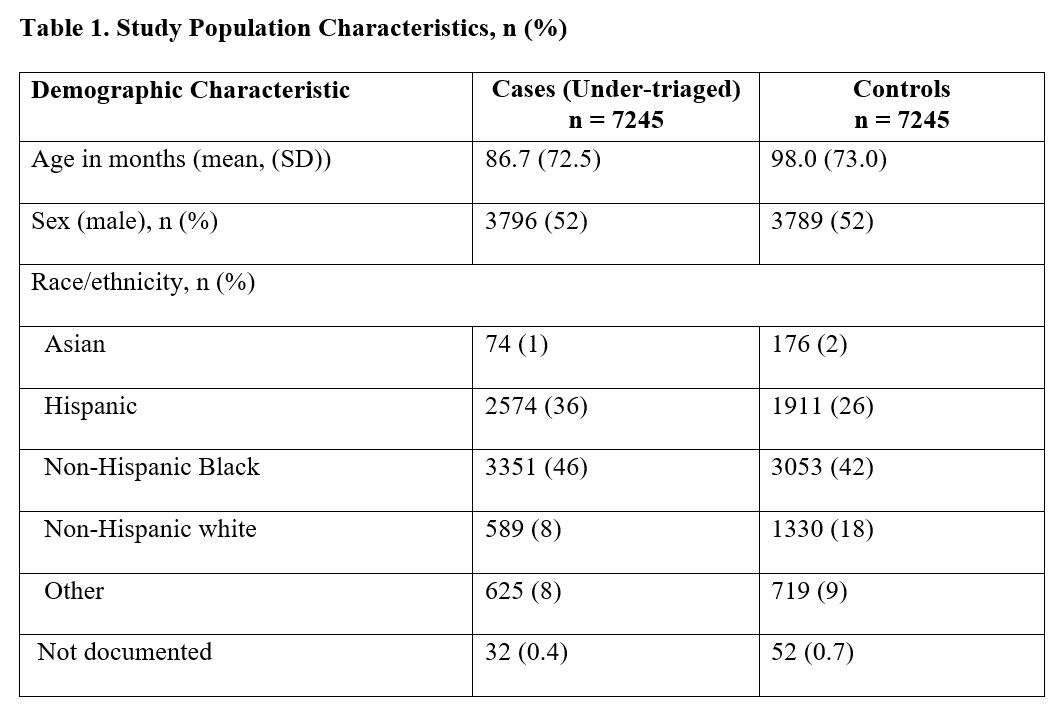
Design/Methods: We defined under-triage as an encounter in which the patient was assigned an Emergency Severity Index (ESI) score of 4 or 5, but subsequently required hospital admission or significant emergency department (ED) resources, including nebulized treatment, supplemental oxygen, or intravenous (IV) line placement. We performed a retrospective study of under-triaged patients 21 years of age and under presenting from January 1, 2018, to January 30, 2022; these constituted cases. Controls were sampled from a pool of ESI 3 patients matched on date, hour of arrival, and intervention received.
Results:
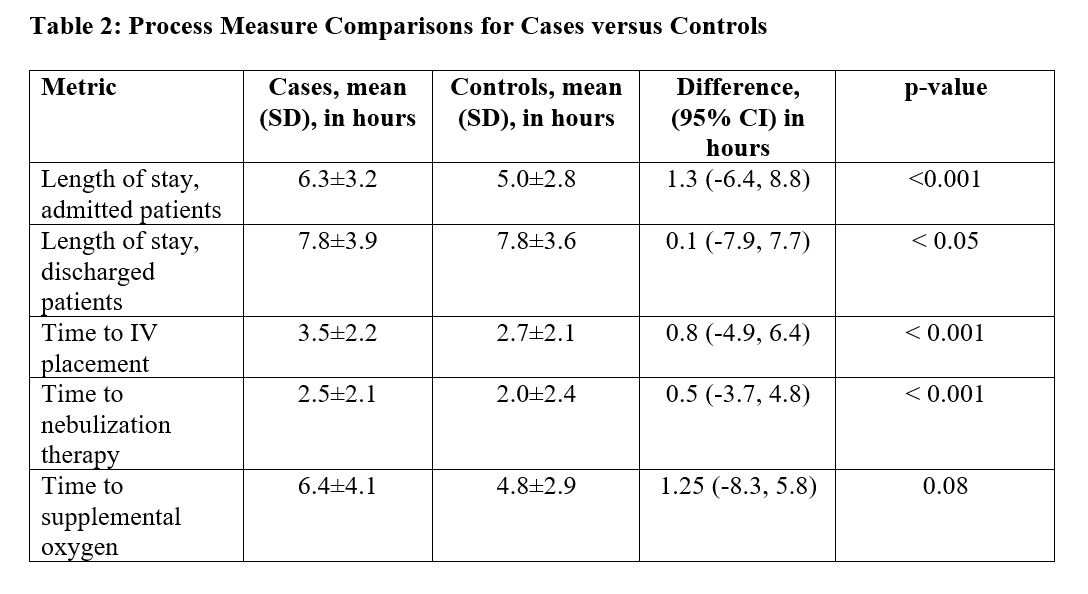
There were 348,899 patients who presented to the ED during the study period, of whom 186,293 (53%) were triaged as ESI 4 or 5. Of these, 7,245 (4%) met the under-triage inclusion criteria; 6,888 (95%) were ESI 4 and 357 (5%) were ESI 5 (Table 1). The mean length of stay for admitted patients was 6.3 hours [standard deviation (SD) 3.2] for cases and 5.0 hours (SD 2.8) hours for controls (p < 0.001). Mean time to IV line placement was 3.5 hours (SD 2.2) for cases compared to 2.7 hours (SD 2.1) for controls (p< 0.001). Mean time to nebulization therapy was 2.5 hours (SD 2.1) compared to 2 hours (SD 2.4) for controls (p < 0.001). Mean time to supplemental oxygen delivery was not statistically significant (Table 2).
Conclusion(s): Under-triaged patients wait longer for admission to the hospital, IV fluids, and nebulized treatments. This is the first study to quantify the clinical impact of under-triage on process measures of care in the pediatric ED and presents an opportunity to improve quality of care in the ED.