Neonatal Quality Improvement
Neonatal Quality Improvement 5
195 - A multicenter quality improvement project to decrease antibiotic utilization rate in very low birth weight infants
Publication Number: 195.439

Stefania Vedovato (she/her/hers)
MD
San Bortolo Hospital of Vicenza
Vicenza, Veneto, Italy
Presenting Author(s)
Background:
Antibiotics are the most prescribed medications in neonatal intensive care units: up to 35-50% of preterm infants receive antibiotics within the first few days of life as prophylaxis for early onset sepsis (EOS) and prolonged therapy has been reported in up to 26% of total antibiotic use, despite negative cultures. Antibiotic overuse has been associated to serious adverse short and long outcomes including late onset sepsis (LOS).
Objective:
Within a multiphase quality improvement project to decrease late onset sepsis in very low birth weight infants (VLBWI), the first main driver was to decrease prophylactic antibiotic therapy at birth.
Design/Methods:
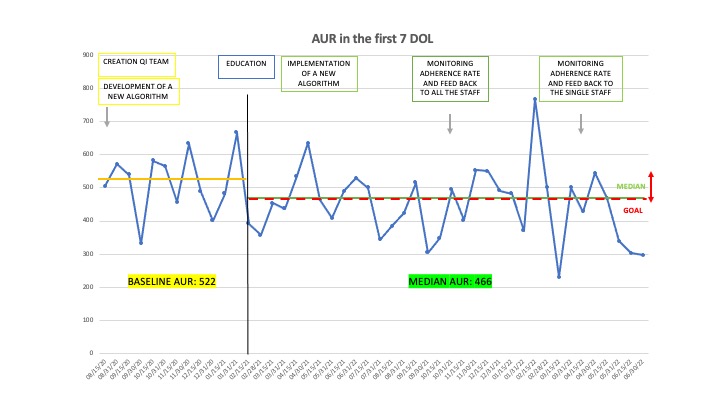
This is a multicenter quality improvement (QI) project, including VLBWI born in 6 III-IV level centers in Triveneto region (Italy), starting in February 2020 with the first objective to achieve a 10-20% reduction in Antibiotic Utilization Rate (AUR) in the first 7 days of life, by June 2022. This initiative was implemented through the following Plan-Do-Study-Act cycles: 1. Creation of a multidisciplinary antibiotic stewardship QI team, definition of a specific aim and definition of QI key measures (February-April 2020); 2. Development of algorithm for evaluation and management of EOS: when to start and when to stop antibiotic therapy, emphasizing the value of negative blood culture at 36-48 hours to discontinue it (May-July 2020); 3. Prospective evaluation of baseline AUR performed every 2 weeks for 6 months (August 2020-January 2021); 4. Education of house staff and nurses through multiple meetings (February 2021); 5. Prospective evaluation of AUR performed every 2 weeks after implementation of the algorithm and evaluation of the rate adherence to it (March 2021-June 2022); 6. Presentation of sequential data to staff using run chart.
Results:
Five hundred and eleven VLBW were included in the project: 144 in the first phase and 368 in the second phase. The two groups were comparable for birth weight (1081+310 g vs 1057+313 g; p > 0,05) and for gestational age (28,8+3,0 wks vs 28,8+2,8 wks; p > 0,05). The overall AUR of the first 7 days of life decreased from 522,8 to 466,8 (10% decreased) and in 5/6 centers AUR decreased from 10 to 61%. The rate of adherence to the new algorithm was 79% to start and 57% to discontinue antibiotic therapy.
During the QI project, no critical events related to missed or delayed identification and treatment of sepsis were reported.
Conclusion(s):
This multicenter QI project was able to decrease AUR in the first 7 days of life in VLBWI. The impact of this single action on decreasing late onset sepsis remains to be determined. .jpg)