Emergency Medicine: All Areas
Emergency Medicine 11
480 - Prehospital expert teleconsultation for critically ill children: A cross-sectional survey of Massachusetts paramedics to identify predictors of adoption
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 480
Publication Number: 480.31
Publication Number: 480.31
Aisling Wright, Boston Medical Center, Boston, MA, United States; H. Holly Hackman, formerly with Boston Medical Center, Providence, RI, United States; Sorraya Jaiprasert, Commonwealth of Medicine, Waltham, MA, United States; Howard J. Cabral, Boston University School of Public Health, Boston, MA, United States; Carlos A. Camargo, MGH/Harvard, Boston, MA, United States; James Feldman, Boston University School of Medicine, Boston, MA, United States; Tehnaz P. Boyle, Boston University School of Medicine, Boston, MA, United States

Aisling Wright (she/her/hers)
Pediatric Emergency Medicine Fellow
Boston Medical Center
Boston, Massachusetts, United States
Presenting Author(s)
Background: Expert teleconsultation via video can improve prehospital outcomes for adults but is underused for children. Understanding predictors of prehospital adoption could promote future use.
Objective: Identify predictors of adoption of pediatric expert teleconsultation by paramedics.
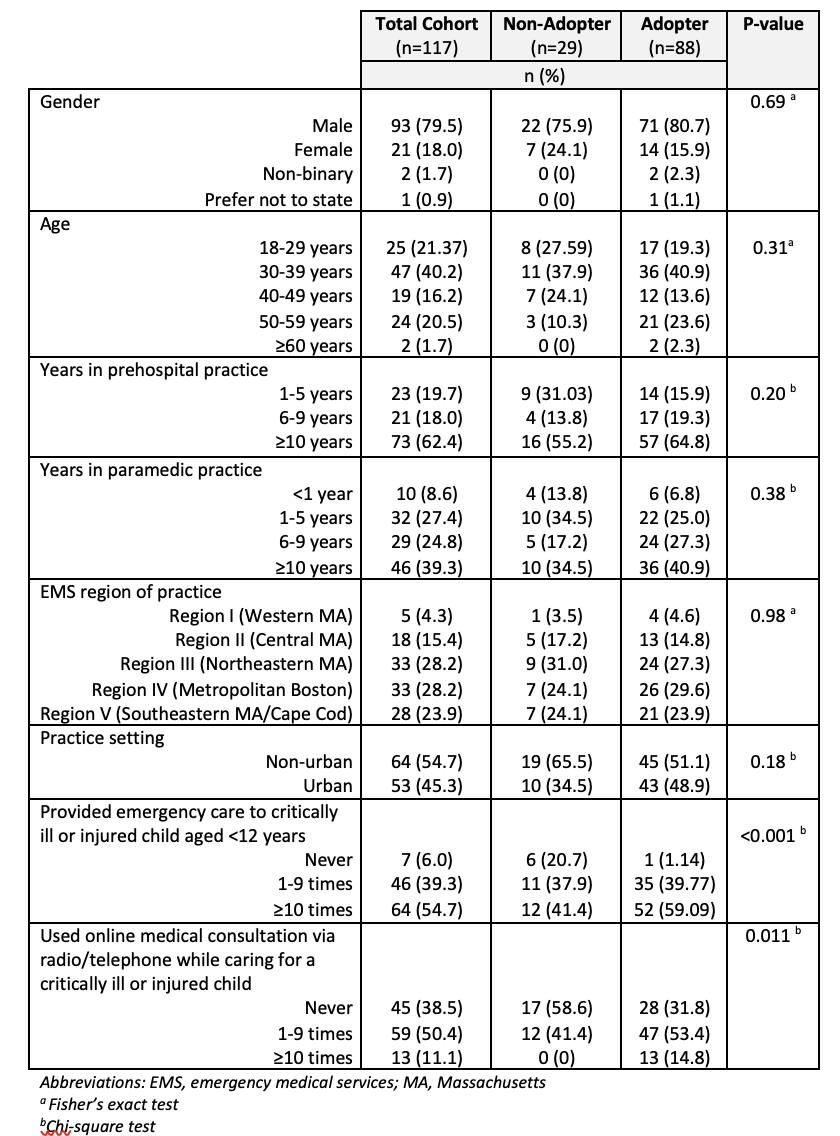
Design/Methods: We used the Technology Acceptance Model to develop a 23-item survey about demographics, experience with children and teleconsultation, perceptions of teleconsultation utility, concerns with use, technology preferences, and intention for future use (adoption). We gave paper or online surveys to Massachusetts paramedics at continuing education offerings (October-December 2021). Participation was voluntary and remunerated. We defined adopters as those reporting future intent to use teleconsultation (primary outcome). We used descriptive statistics; Chi-square or Fisher’s exact tests for associations between age, gender, years in practice, practice setting, and clinical experience and adoption; and logistic regression to estimate the odds of adoption given paramedics’ opinion that teleconsultation would improve outcomes.
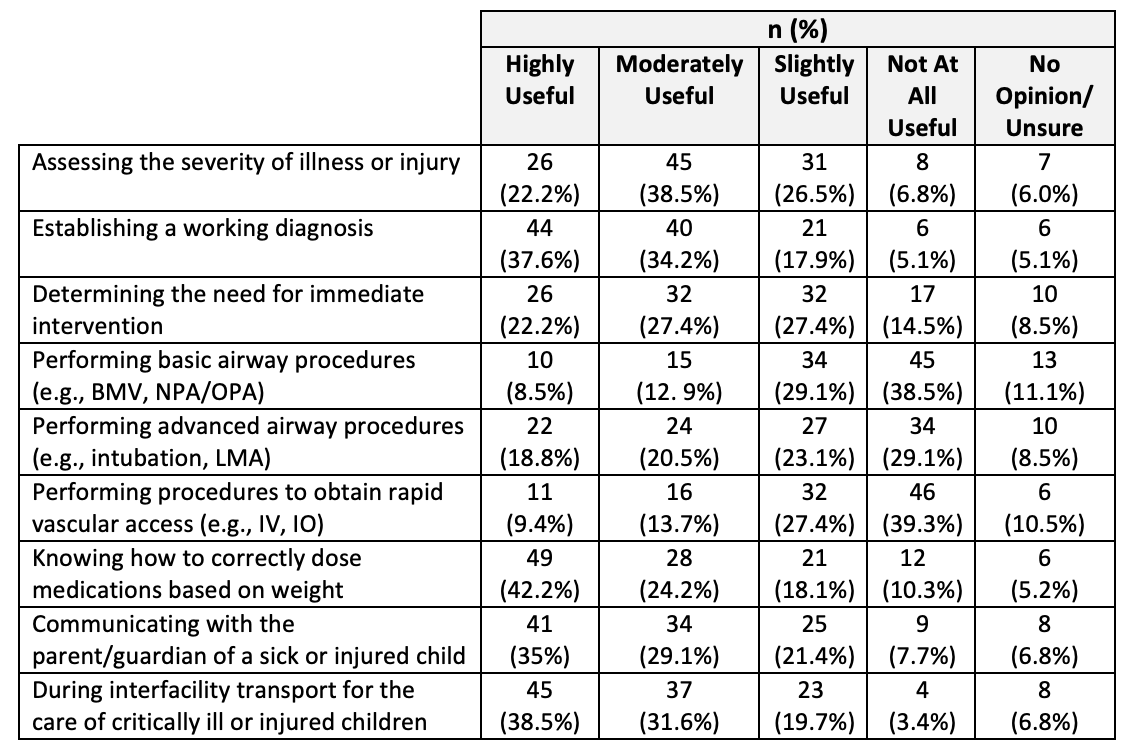
Results: Of 167 paramedics in attendance, 117 participated (70% response). Half (50%) felt current protocols with medical consultation via radio were sufficient. Only 12% had ever used expert teleconsultation via video, and only for adults. Still, 90% believed pediatric expert teleconsultation would improve outcomes and 75% were adopters. Table 1 reports the association between participant demographics and adoption. Agreement that expert teleconsultation would improve outcomes was associated with odds of adoption (OR 23.1, p < 0.001) even after adjusting for practice setting and years of experience. Perceived utility was greatest for patient assessment, medication dosing, communication and interfacility transport, and least for procedures (Table 2). Time delays from equipment use (47%) or teleconsultation (63%), broadband access (54%), and lack of teleconsultant knowledge of EMS protocols or scope of practice (47%) were leading concerns. Cost (9%), privacy (9%), and liability (5%) concerns were infrequent. Most preferred hands-free (82%), portable (73%) devices.
Conclusion(s): Massachusetts paramedics indicated pediatric expert teleconsultation could improve outcomes and be useful for non-procedural care delivery. We encourage system developers to minimize time delays and use reliable broadband and well-trained teleconsultants. Future research will need to demonstrate prehospital efficacy of teleconsultation for children to promote widespread adoption.