Back
Background: Cardiorespiratory deterioration is common in very low birth weight (< 1500g) infants. This period of critical brain growth and development may be impacted by insults such as sepsis and hypoxia. The physiological response to illness manifests through autonomic signaling and is detected as changes in heart rate (HR) and oxygenation (SpO2). We hypothesize that limited autonomic activity and reactivity may indicate poor cardiovascular autoregulation, increasing the risk of cerebral hypoxic-ischemia, the fundamental basis for preterm brain injury, and is correlated with decreased brain growth at term equivalent age (TEA).
Objective: Test the hypothesis that cumulative cardiorespiratory signatures of illness predict TEA brain volumes.
Design/Methods: Preterm infants born < 32 weeks were prospectively recruited for a longitudinal pilot study including longitudinal HR/SpO2 data collection and a TEA brain MRI.
Cardiorespiratory stability was quantified using a validated multi-feature logistic regression model called pulse oximetry warning score (POWS). Recordings were segmented into 10-minute windows, error-corrected, and seven different metrics calculated: 3 from the HR signal, 3 from the SpO2 signal, and one from a combination of the HR and SpO2 (maximum positive value of the cross correlation). The mean and standard deviation (SD) of the 10-minute POWS scores were calculated over the course of the entire NICU stay, where a low mean POWS represents decreased activity and low SD POWS represents decreased reactivity.
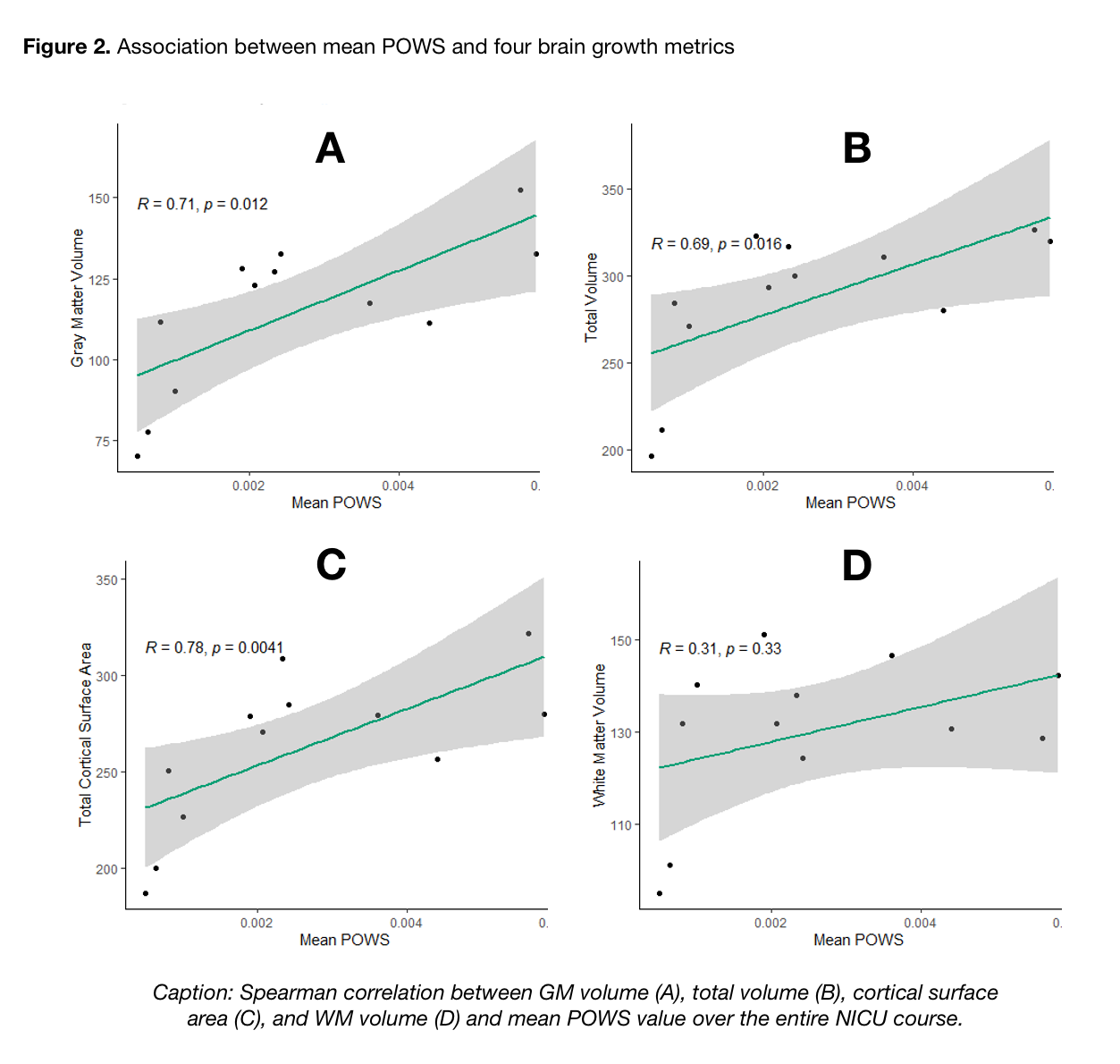
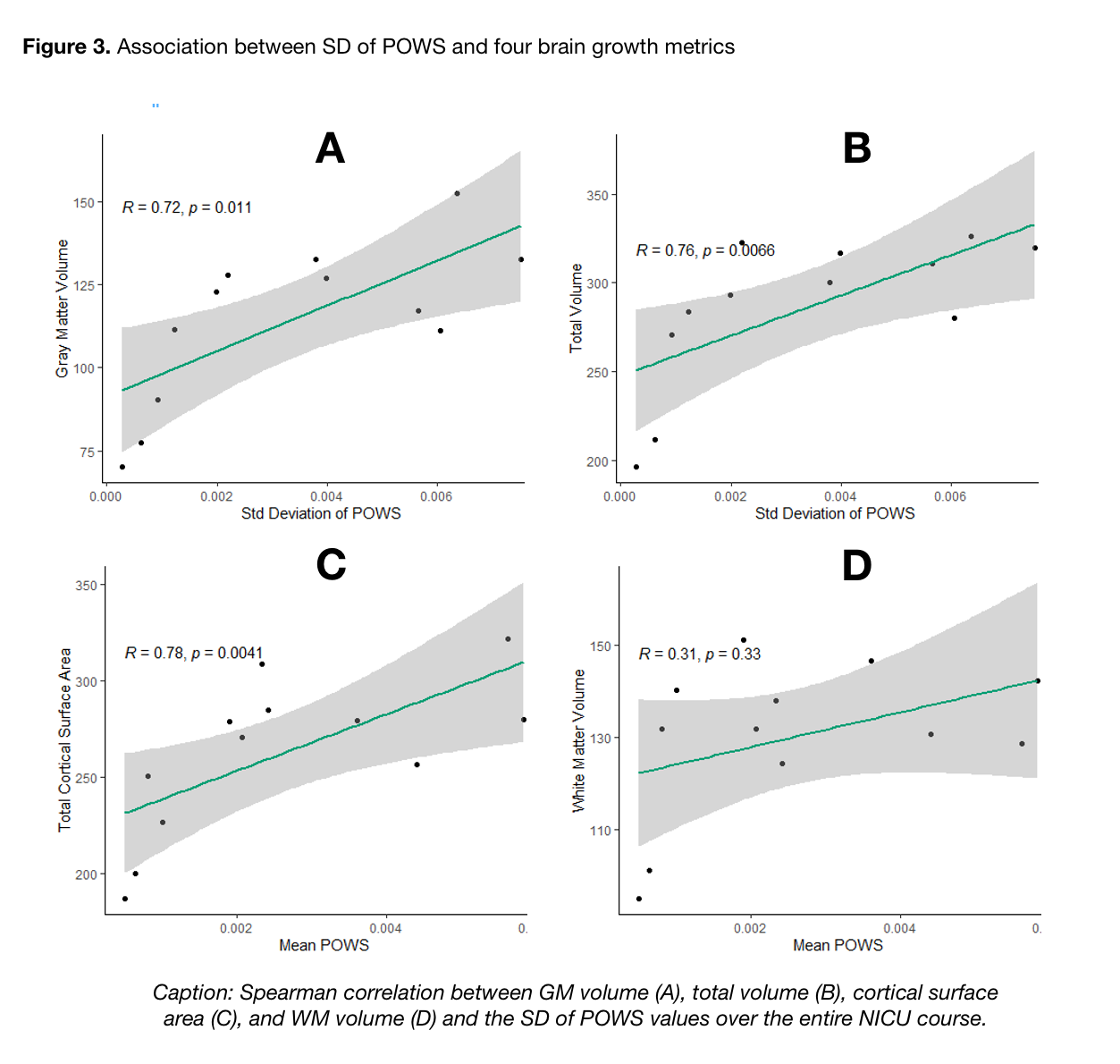
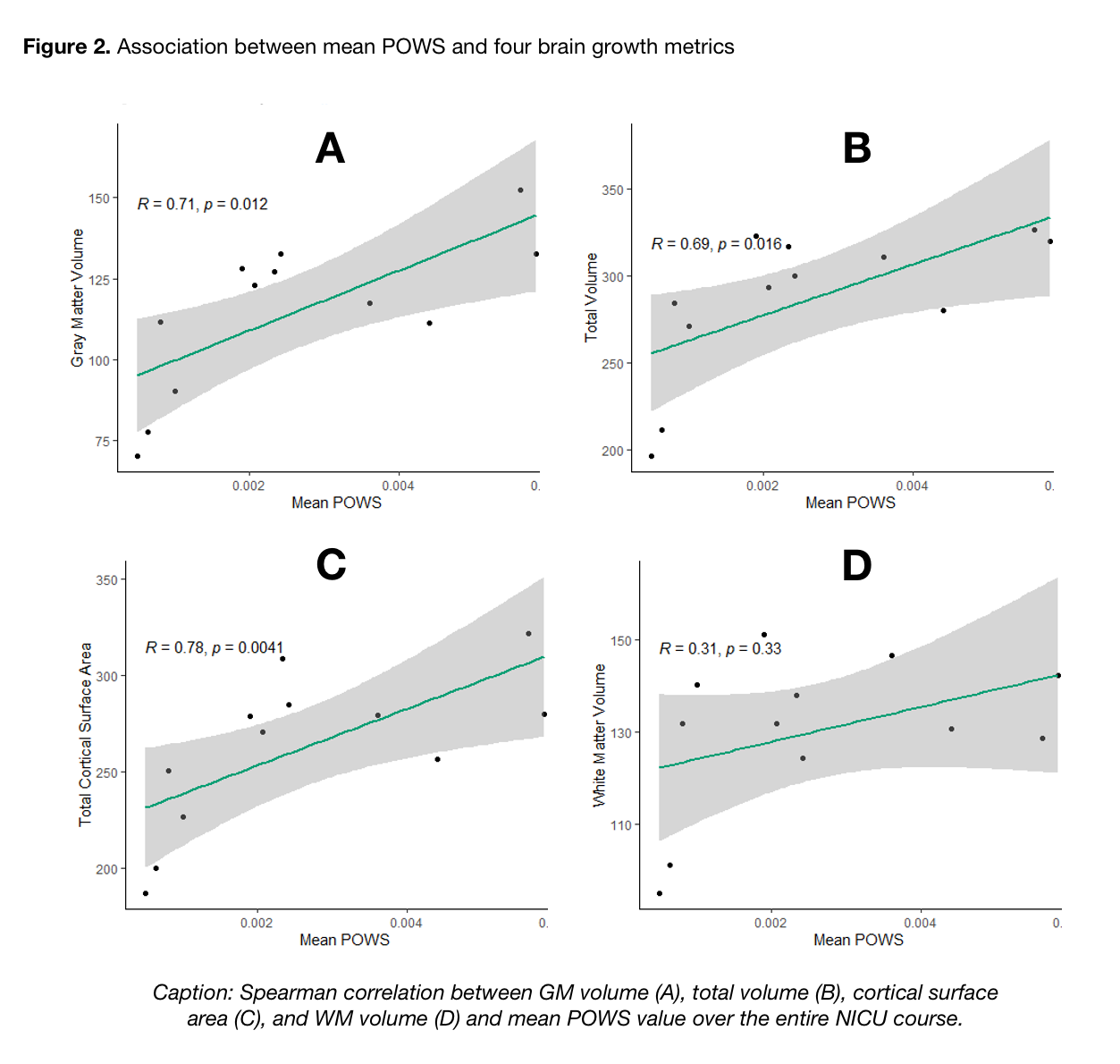
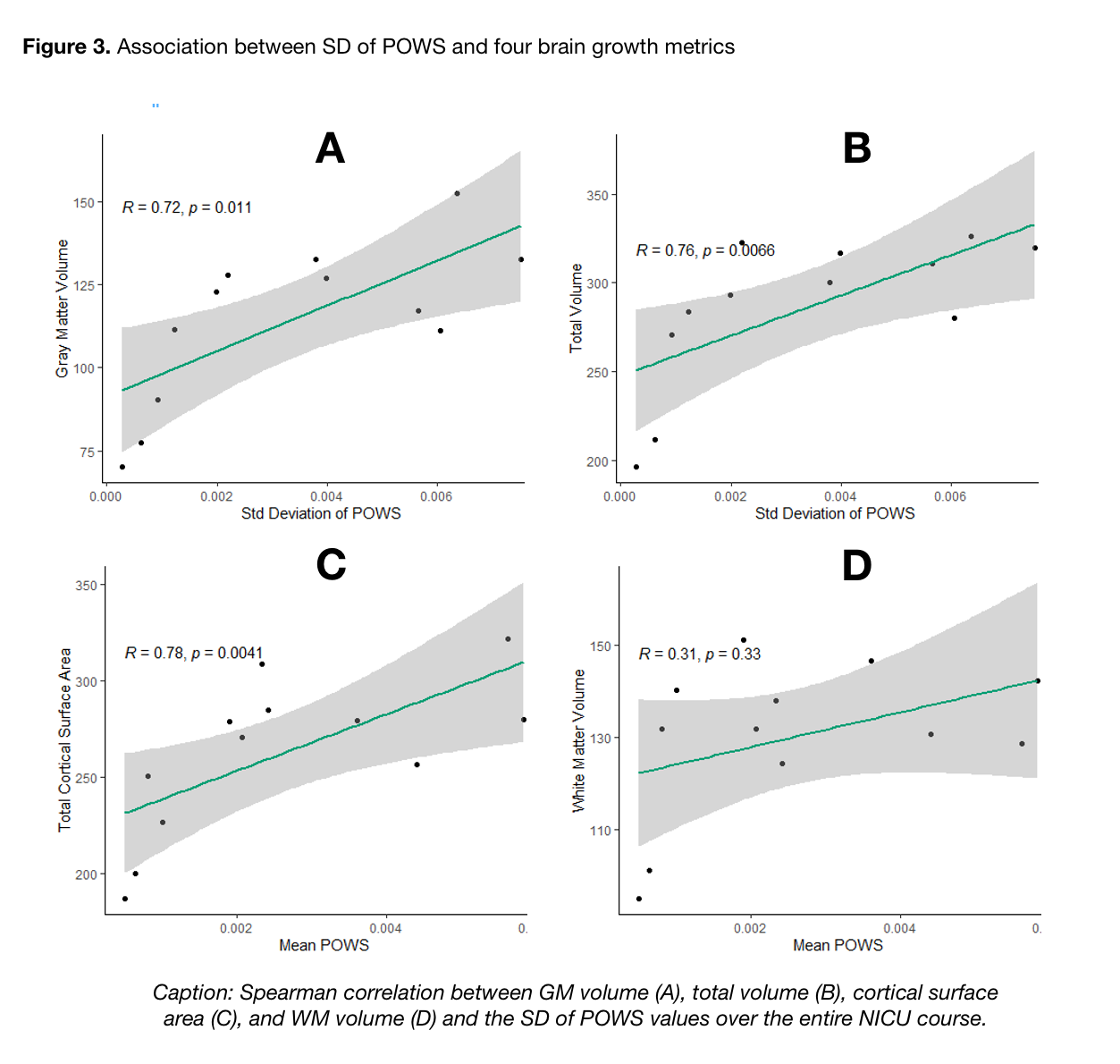
Using T2W images, total cortical surface area (CSA), gray matter, white matter, and total brain volume were calculated using a semi-automated pipeline. We used Spearman correlation to evaluate the relationship between the mean and SD of POWS with brain volumetrics.
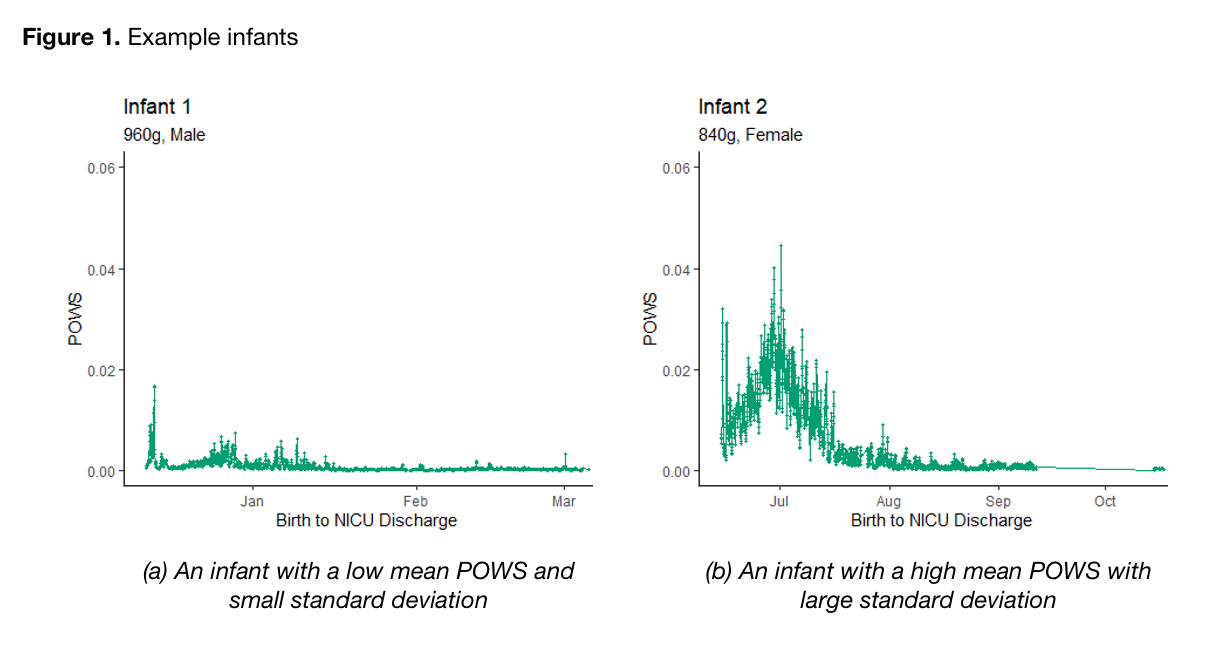
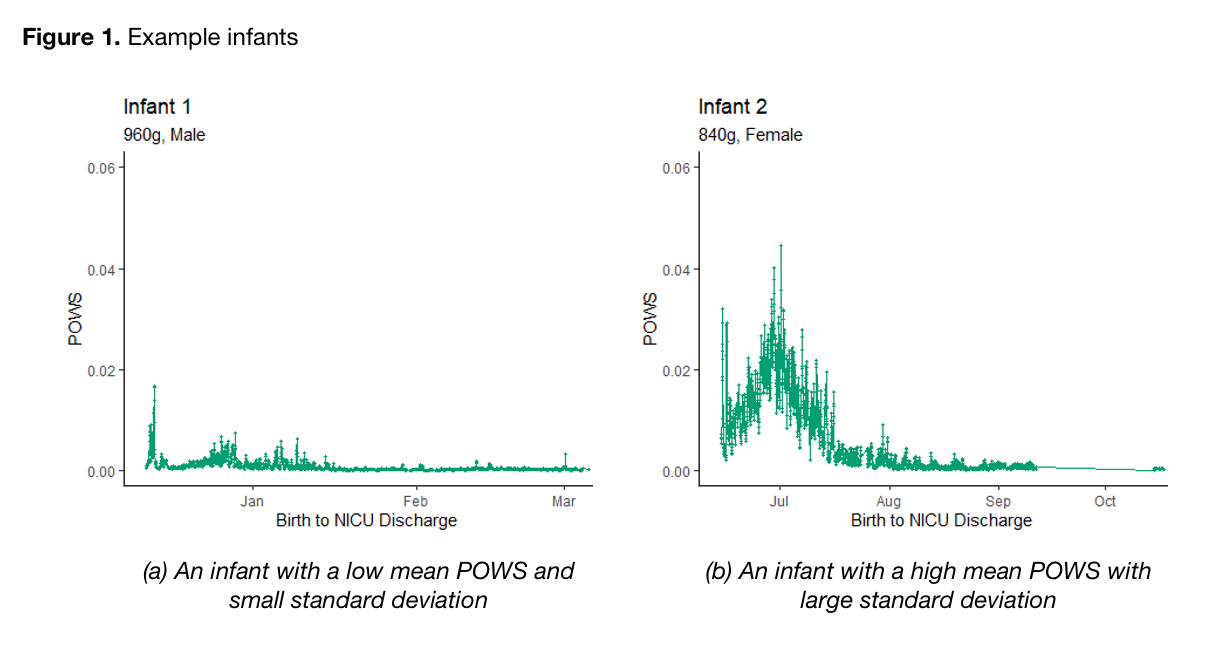
Results: As shown in Figure 1, marked differences in autonomic activity (mean POWS) and reactivity (SD POWS) are readily apparent between infants. A higher mean POWS during NICU hospitalization was associated with increased gray matter volume (r = 0.71, p = 0.01), total brain volume (r = 0.69, p = 0.02), and cortical surface area (r = 0.78, p< 0.01). As shown in Figure 3, an even stronger association was noted between SD POWS and gray matter volume (r = 0.72, p = 0.01), total brain volume (r = 0.76, p< 0.01), and cortical surface area (r = 0.78, p< 0.01).
Conclusion(s): Autonomic activity and reactivity, expressed through mean and SD POWS scores, were strongly correlated with greater brain growth at TEA in preterm infants. These results generate hypotheses that warrant further study as potential tools to predict neurologic outcomes.
Neonatal Neurology: Clinical Research
Neonatal Neurology 5: Clinical
114 - Cardiorespiratory instability and reactivity correlate with brain volume at term-equivalent age in very low birth weight infants
Sunday, April 30, 2023
3:30 PM – 6:00 PM ET
Poster Number: 114
Publication Number: 114.337
Publication Number: 114.337
Zachary A. Vesoulis, Washington University School of Medicine, St. Louis, MO, United States; Sherry L. Kausch, University of Virginia School of Medicine, Charlottesville, VA, United States; Dimitrios Alexopoulos, Washington University in St. Louis School of Medicine, St. Louis, MO, United States; Christopher D. Smyser, Washington University in St. Louis, St. Louis, MO, United States; Brynne A. Sullivan, University of Virginia School of Medicine, KESWICK, VA, United States

Zachary A. Vesoulis, MD MSCI (he/him/his)
Assistant Professor
Washington University School of Medicine
St. Louis, Missouri, United States
Presenting Author(s)
Background: Cardiorespiratory deterioration is common in very low birth weight (< 1500g) infants. This period of critical brain growth and development may be impacted by insults such as sepsis and hypoxia. The physiological response to illness manifests through autonomic signaling and is detected as changes in heart rate (HR) and oxygenation (SpO2). We hypothesize that limited autonomic activity and reactivity may indicate poor cardiovascular autoregulation, increasing the risk of cerebral hypoxic-ischemia, the fundamental basis for preterm brain injury, and is correlated with decreased brain growth at term equivalent age (TEA).
Objective: Test the hypothesis that cumulative cardiorespiratory signatures of illness predict TEA brain volumes.
Design/Methods: Preterm infants born < 32 weeks were prospectively recruited for a longitudinal pilot study including longitudinal HR/SpO2 data collection and a TEA brain MRI.
Cardiorespiratory stability was quantified using a validated multi-feature logistic regression model called pulse oximetry warning score (POWS). Recordings were segmented into 10-minute windows, error-corrected, and seven different metrics calculated: 3 from the HR signal, 3 from the SpO2 signal, and one from a combination of the HR and SpO2 (maximum positive value of the cross correlation). The mean and standard deviation (SD) of the 10-minute POWS scores were calculated over the course of the entire NICU stay, where a low mean POWS represents decreased activity and low SD POWS represents decreased reactivity.
Using T2W images, total cortical surface area (CSA), gray matter, white matter, and total brain volume were calculated using a semi-automated pipeline. We used Spearman correlation to evaluate the relationship between the mean and SD of POWS with brain volumetrics.
Results: As shown in Figure 1, marked differences in autonomic activity (mean POWS) and reactivity (SD POWS) are readily apparent between infants. A higher mean POWS during NICU hospitalization was associated with increased gray matter volume (r = 0.71, p = 0.01), total brain volume (r = 0.69, p = 0.02), and cortical surface area (r = 0.78, p< 0.01). As shown in Figure 3, an even stronger association was noted between SD POWS and gray matter volume (r = 0.72, p = 0.01), total brain volume (r = 0.76, p< 0.01), and cortical surface area (r = 0.78, p< 0.01).
Conclusion(s): Autonomic activity and reactivity, expressed through mean and SD POWS scores, were strongly correlated with greater brain growth at TEA in preterm infants. These results generate hypotheses that warrant further study as potential tools to predict neurologic outcomes.