Neonatal Quality Improvement
Neonatal Quality Improvement 4
743 - Quality Improvement Project to Improve Compliance with Hand Hygiene in a Level III NICU
Publication Number: 743.343

Pavani Chitamanni, MBBS (she/her/hers)
Resident Physician
State University of New York Downstate Medical Center College of Medicine
Brooklyn, New York, United States
Presenting Author(s)
Background:
Healthcare-Associated-Infections (HAIs) are one of the most common complications of healthcare, with a huge economic impact. They cause significant morbidity and mortality in the Neonatal Intensive Care Units (NICU). Hand hygiene (HH) is a simple and effective measure to decrease these infections.
Objective:
To improve HH compliance in the NICU at NYC Health + Hospitals, Kings County, by 20% within a six-month period, from October 1st, 2022 to March 31st, 2023.
Design/Methods:
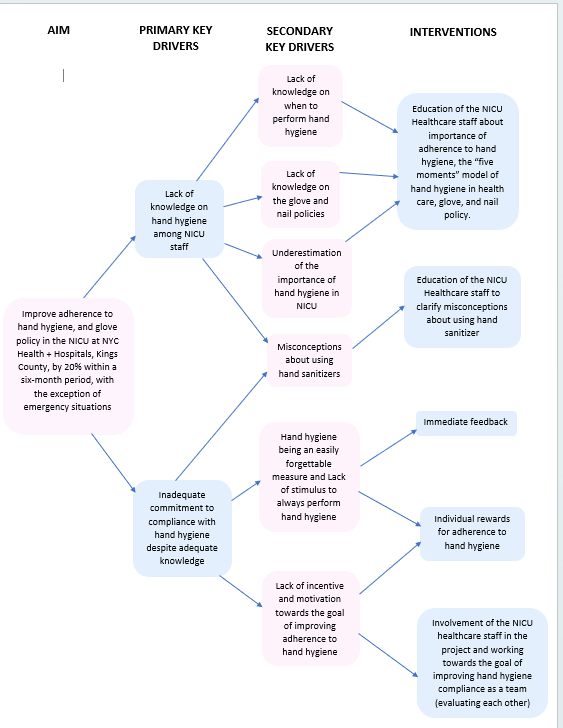
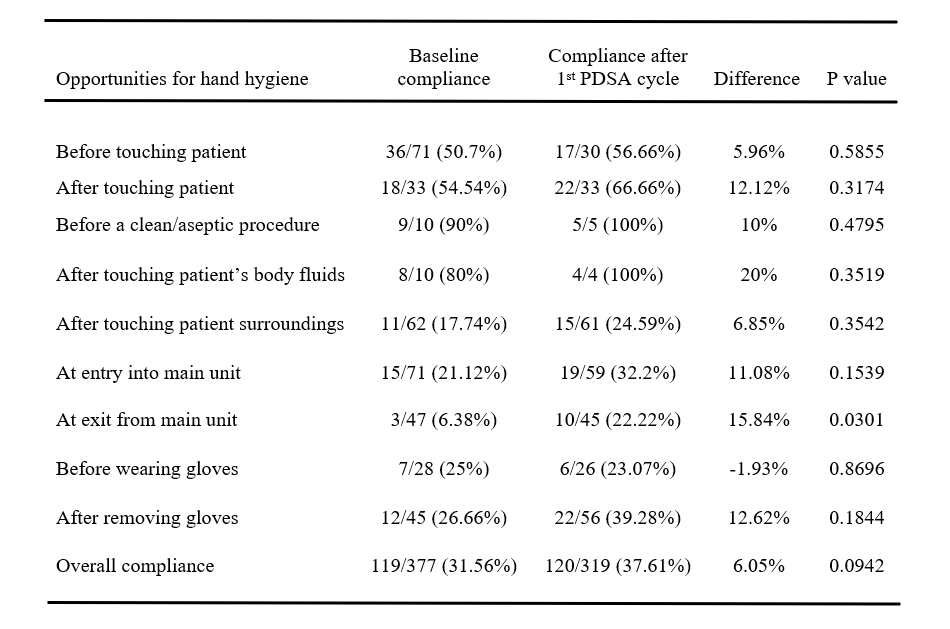
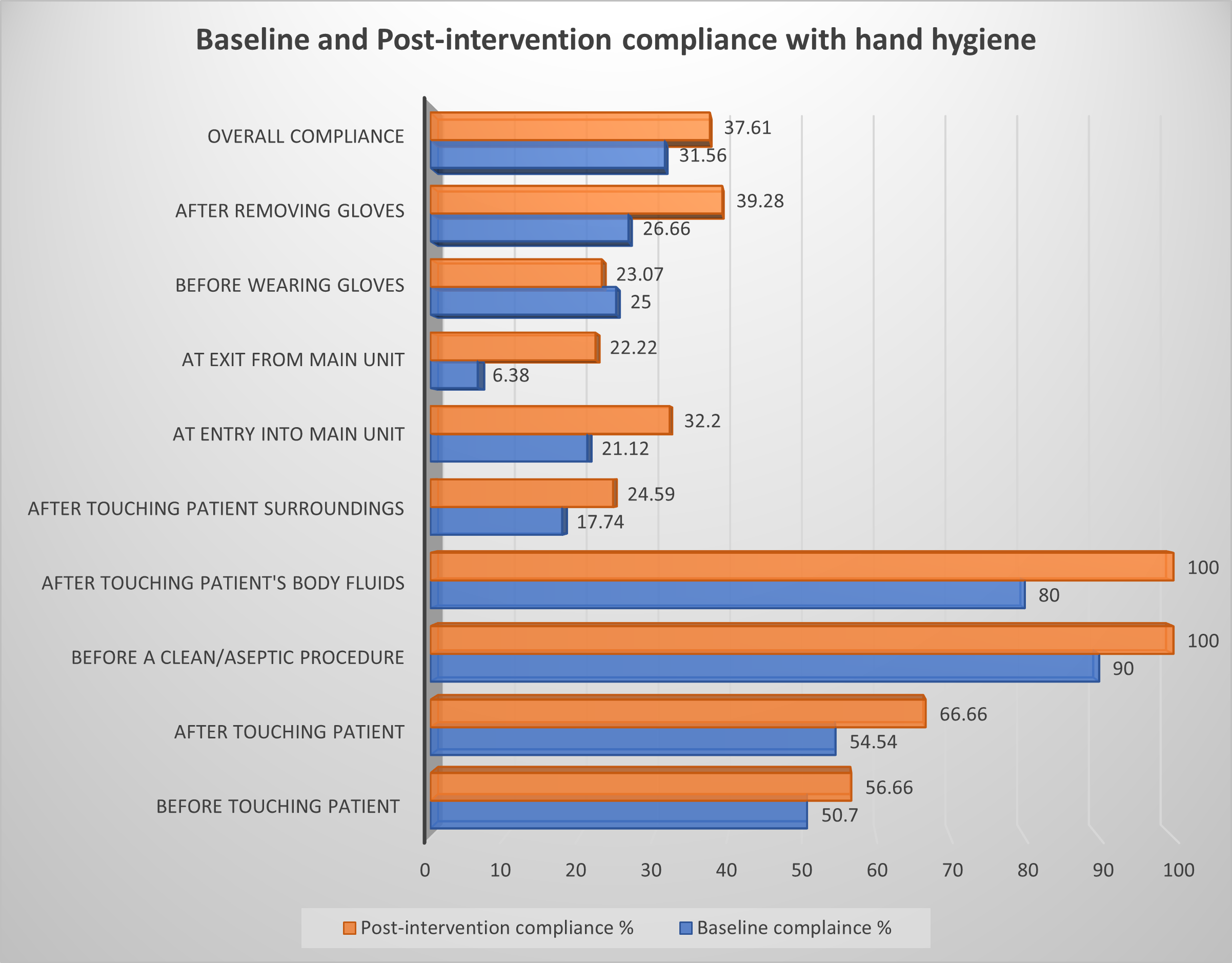
The QI Model for Improvement (Figure 1) was used to guide our interventions. HH compliance in the unit was assessed by covert observations of the Health Care Workers (HCW) including physicians, nurses and respiratory therapists. Compliance was calculated as number of times HH performed per total number of HH opportunities. Nine HH opportunities were observed: a) before touching patient b) after touching patient c) before a clean/aseptic procedure d) after body fluid exposure e) after touching patient surroundings f) at entry into unit g) at exit from unit h) before wearing gloves i) after wearing gloves. Baseline compliance at these opportunities ranged from 6% to 90%, with notably low compliance at 5 out of the 9 HH opportunities (Table 1). These were addressed through HCW education using the “five moments” model, discussions on the importance and misconceptions of HH, and the glove and nail policies. Individual surveys were conducted among the staff to assess the knowledge, perceptions, and barriers to HH. The outcome measure for this QI project was the compliance percentage, while the process measure was the number of educational interventions such as presentations and emails. The balancing measure was perceived increase in work burden and interference with patient care. The chi-squared test for proportions was used for analysis.
Results:
We had a total of 377 observations at baseline and 319 observations for the first PDSA cycle. The baseline compliance was 31.56%. After the first intervention, there was a 6% increase in overall compliance, with improvement ranging from 5.96% to 20% at the nine hand hygiene opportunities (Table 1, Figure 2). The median self-reported compliance by HCWs was >80% on individual surveys. Common barriers to HH identified were increased work burden (83.3%), skin dryness and irritation (66.7%) and empty or broken sanitizer dispensers (66.7%).
Conclusion(s):
This QI initiative increased HH compliance in our NICU by 6% after one PDSA cycle. Further cycles are in progress to reach the target of a 20% increase. They are directed at inadequate commitment to compliance, despite adequate knowledge.