Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 2: Physiology 1
333 - Non-Invasive Neurally-Adjusted Ventilatory Assist Decreases pCO2 in Extubated Premature Infants
Publication Number: 333.345

Rawan Al-Rawi, MBBS (she/her/hers)
Pediatric Resident
University of Iowa Roy J. and Lucille A. Carver College of Medicine
Iowa City, Iowa, United States
Presenting Author(s)
Background:
Preterm infants often require mechanical ventilatory support, but prolonged endotracheal intubation is associated with airway injury, bronchopulmonary dysplasia (BPD), and developmental impairment. Non-invasive methods to assist ventilation in this population are needed. Non-invasive neurally adjusted ventilatory assist (NIV-NAVA) provides synchronized ventilatory support via measurement of diaphragm electrical activity, but prospective studies are limited in preterm infants.
Objective: To measure the efficacy of ventilation support of synchronized noninvasive ventilation via neurally adjusted ventilatory assist (NIV NAVA) in post-extubated premature infants via comparison of pre-and-post-NAVA capillary pCO2 and pH.
Design/Methods:
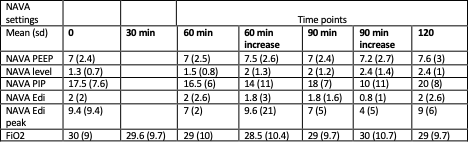
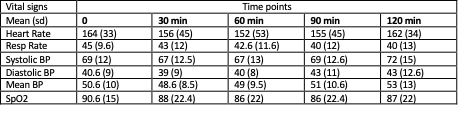
Prospective cross-over trial of preterm infants treated with surfactant for respiratory distress syndrome. Infants < 1500 g birthweight, > 7d of age, and extubated > 48 hours on stable CPAP were included. Parents provided informed consent. Infants were placed on NAVA support at stable PEEP with NAVA (cm H30/mV) level increased by 50% q 30min x 3. Capillary blood gas before and after 120 min study period were compared. Heart rate (HR), respiratory rate (RR), SpO2, blood pressure (BP), FiO2, and ventilator settings were measured q 30min. Transcutaneous CO2 monitoring was used for safety. Wilcoxon signed-rank test was used to compare pH, pCO2, and vital signs before and after intervention. Repeated-measures ANVOA was used to assess changes in HR, RR, BP, SpO2, FiO2, and ventilator settings across 4 study time points. SAS 9.4 was used for analysis.
Results: 29 infants were studied, mean gestational age 25 weeks (± 2.02 sd), mean post-menstrual age at study 32 weeks (± 3.5 sd). Mean PEEP was 7.5 cmH20 (±3 sd), FiO2 0.32 (± 0.16). HR, RR, BP, SpO2 were not affected by NAVA intervention. Mean pCO2 decreased after NAVA (-2.2 mmHg (±3sd), p = 0.02), pH increased (+0.02 (± 0.04 sd, p = 0.03). HR, RR, FiO2 and SpO2 did not vary during the study period (table 2). Ventilator settings are shown in table 1.
Conclusion(s):
Non-invasive NAVA is effective in decreasing pCO2 and increasing pH in preterm infants on CPAP with a history of mechanical ventilation, without affecting vital signs..png)