Back
Background: The global prevalence of Congenital Heart Disease (CHD) at birth is currently estimated to be 1.8 cases per 100 live births. Critical CHD (CCHD), defined as a case requiring surgical or catheter intervention in the first year of life, occurs in approximately 25% of those with CHD. A large disparity exists in the global capacity to identify and care for these patients. In Colombia, the universal use of pulse oximetry screening 24 hours after birth is recommended by law. However, there is a significant lag in routine adoption of this practice that leads to late or missed diagnoses for CCHD.
Objective: The initiative goal is to impact mortality and morbidity associated with a delayed CCHD diagnosis by accelerating the adoption of routine newborn cardiac screening protocols. The program established an initial goal of screening 100,000 newborns within five years of program launch.
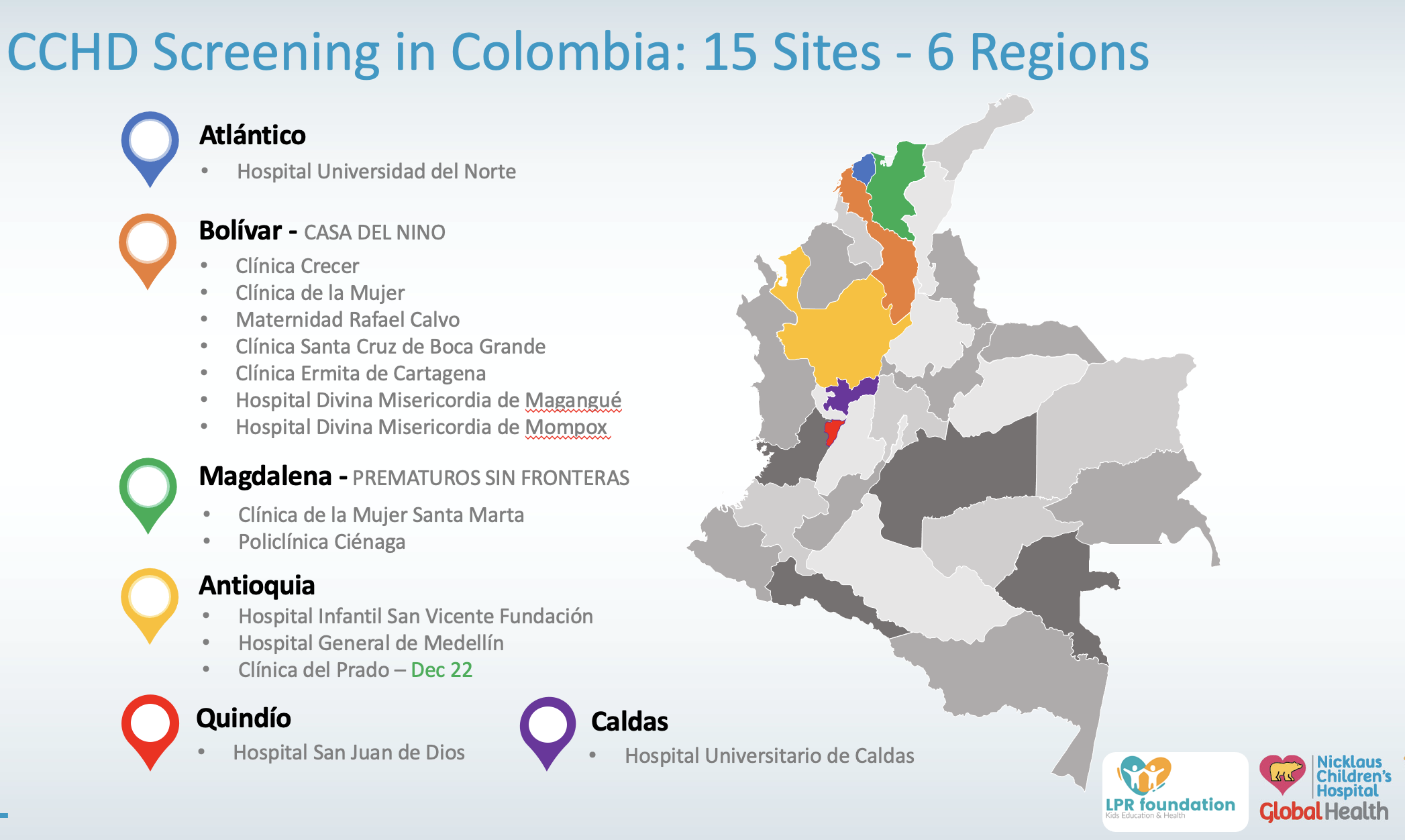
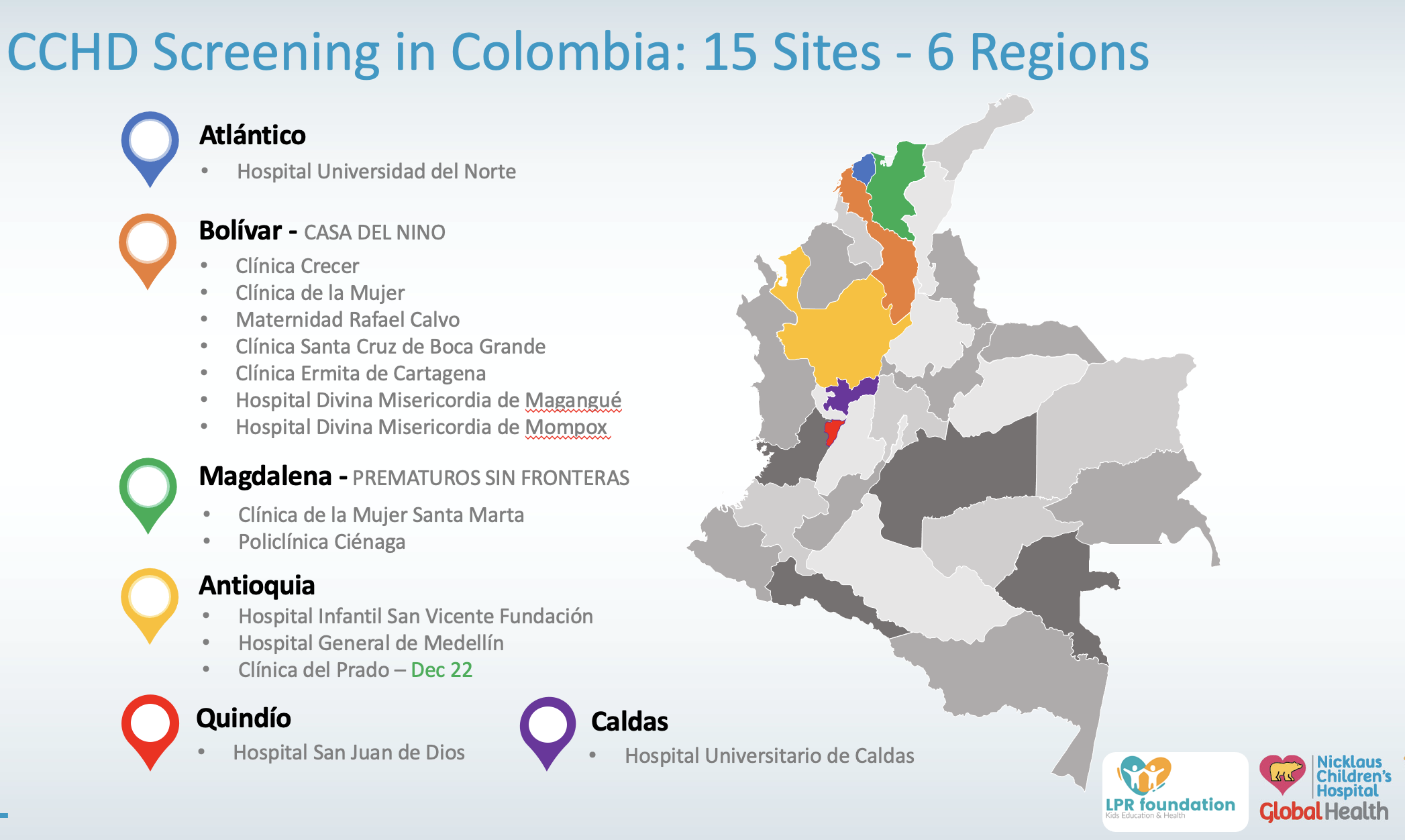
Design/Methods: We deployed an innovative model to enhance access to pediatric cardiovascular care via multisite, multi-city, and multi regional clinical and educational partnerships. The program provided participating sites with the required capital equipment (15 Pulse Oximeters, 6 Echocardiographs), as well as all related educational and technical training (240 nurses and 35 physicians).
We would like to acknowledge the LPR & LDG Foundation for their generous support as a collaborative global health effort with Nicklaus Children's Hospital.
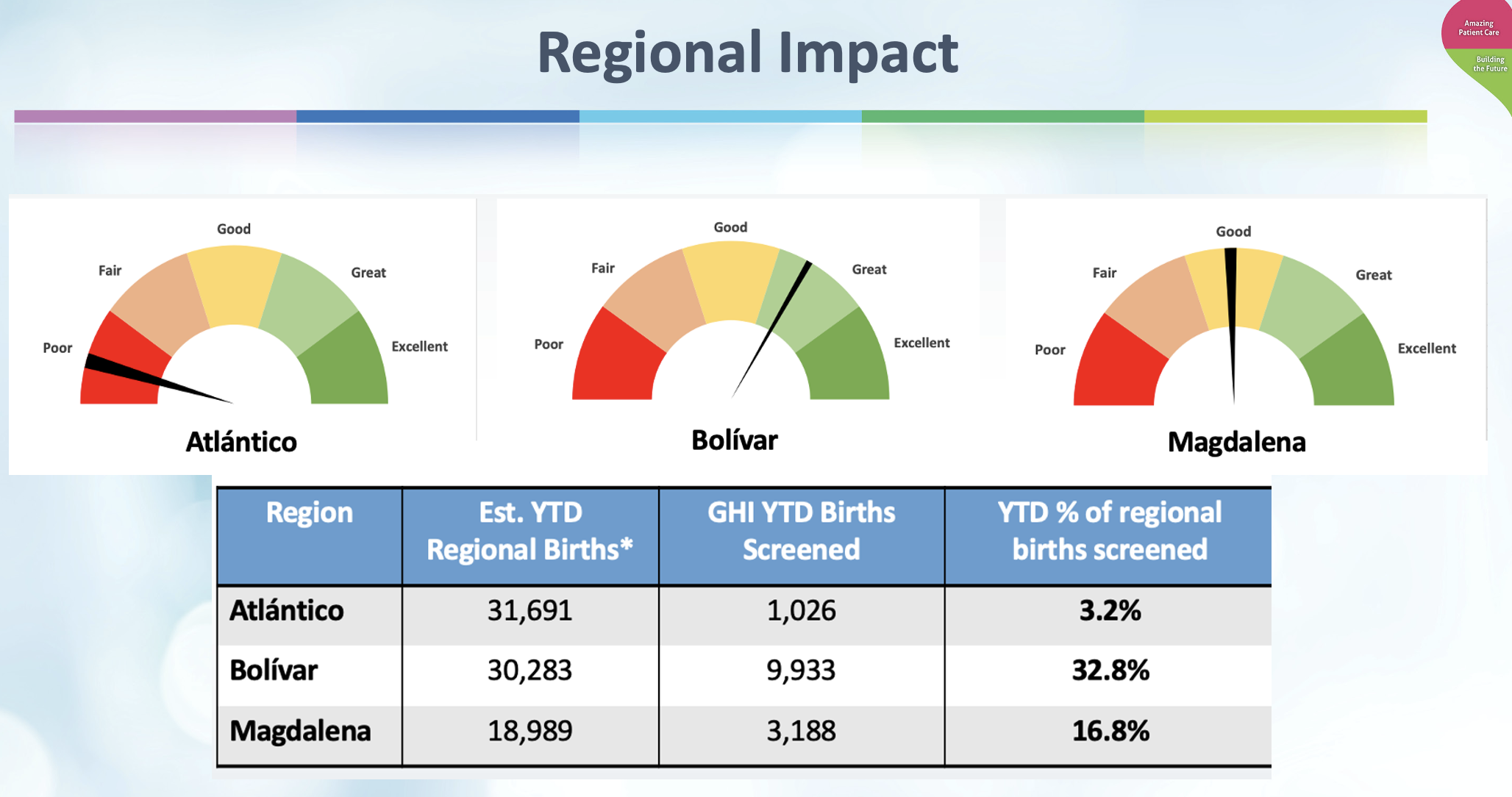
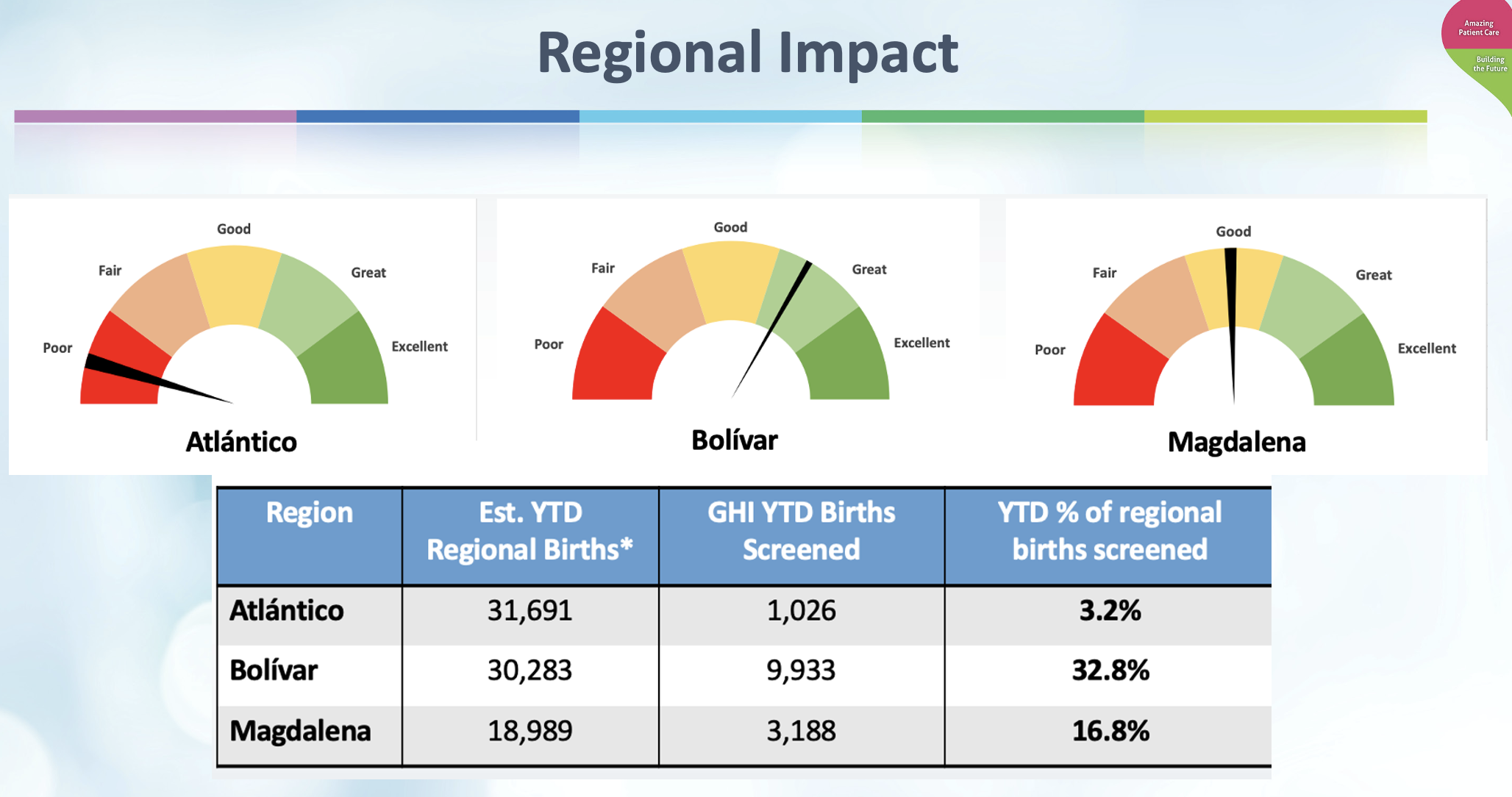
Results: To date we have operationalized 15 screening sites in 6 different regions in Colombia. We have screened more than 37,000 newborns. To date a total of 80 CHD cases were identified, with 13 CCHDs requiring immediate surgical intervention. Our qualitative analysis revealed wide regional impact disparities in patterns of care, and the peculiar challenges of each one of them. The program has also expanded and evolved by establishing a pediatric ECMO center and an Interventional Pediatric Cardiology suite.
Conclusion(s): Universal CCHD screening implementation in Colombia provided significant value for newborns identified with CHD and for others with hypoxemic conditions. Our structured approach successfully addressed and impacted the wide variation in current program adoption observed across different regions. The universal adoption of CCHD screening will not be feasible without further endorsement and support of the government and payor. Our long-term vision is to replicate and scale an optimal program framework to other countries, as well as to expand into other innovative models of pediatric subspecialty care.
Global Neonatal & Children's Health
Global Neonatal & Children's Health 1
626 - Critical Congenital Heart Disease (CCHD) Screening - The Colombia Experience
Sunday, April 30, 2023
3:30 PM – 6:00 PM ET
Poster Number: 626
Publication Number: 626.315
Publication Number: 626.315
Andrea Maggioni, Nicklaus Children’s Hospital, Miami, FL, United States; Sonia Morales, Hospital San Vicente Fundación, Medellin, Antioquia, Colombia; Carolina Jimenez Alvarez, Hospital General de Medellin, Medellin, Antioquia, Colombia; Oscar San Roman, Newborn Foundation, Queretaro, Queretaro de Arteaga, Mexico; Alessandra Maggioni, University of Miami, Miami, FL, United States

Andrea Maggioni, MD PhD MBA (he/him/his)
Director of Global Health
Nicklaus Children’s Hospital
Miami Beach, Florida, United States
Presenting Author(s)
Background: The global prevalence of Congenital Heart Disease (CHD) at birth is currently estimated to be 1.8 cases per 100 live births. Critical CHD (CCHD), defined as a case requiring surgical or catheter intervention in the first year of life, occurs in approximately 25% of those with CHD. A large disparity exists in the global capacity to identify and care for these patients. In Colombia, the universal use of pulse oximetry screening 24 hours after birth is recommended by law. However, there is a significant lag in routine adoption of this practice that leads to late or missed diagnoses for CCHD.
Objective: The initiative goal is to impact mortality and morbidity associated with a delayed CCHD diagnosis by accelerating the adoption of routine newborn cardiac screening protocols. The program established an initial goal of screening 100,000 newborns within five years of program launch.
Design/Methods: We deployed an innovative model to enhance access to pediatric cardiovascular care via multisite, multi-city, and multi regional clinical and educational partnerships. The program provided participating sites with the required capital equipment (15 Pulse Oximeters, 6 Echocardiographs), as well as all related educational and technical training (240 nurses and 35 physicians).
We would like to acknowledge the LPR & LDG Foundation for their generous support as a collaborative global health effort with Nicklaus Children's Hospital.
Results: To date we have operationalized 15 screening sites in 6 different regions in Colombia. We have screened more than 37,000 newborns. To date a total of 80 CHD cases were identified, with 13 CCHDs requiring immediate surgical intervention. Our qualitative analysis revealed wide regional impact disparities in patterns of care, and the peculiar challenges of each one of them. The program has also expanded and evolved by establishing a pediatric ECMO center and an Interventional Pediatric Cardiology suite.
Conclusion(s): Universal CCHD screening implementation in Colombia provided significant value for newborns identified with CHD and for others with hypoxemic conditions. Our structured approach successfully addressed and impacted the wide variation in current program adoption observed across different regions. The universal adoption of CCHD screening will not be feasible without further endorsement and support of the government and payor. Our long-term vision is to replicate and scale an optimal program framework to other countries, as well as to expand into other innovative models of pediatric subspecialty care.