Neonatal Follow-up
NICU Follow Up and Neurodevelopment 5: Impact of Parents and Social Determinants of Health
156 - Parental anxiety after extremely preterm birth and its relationship with neuromotor development and perinatal risk factors
Publication Number: 156.363

Loïs C. Span (she/her/hers)
MD/PhD student
University Medical Center Groningen
Groningen, Groningen, Netherlands
Presenting Author(s)
Background:
Understanding psychological effects of preterm birth on parents after discharge from the NICU is important, because it may impact their well-being and parenting capacity. Prematurity itself can have negative effects on a child's neurodevelopment, but research into the association between postnatal neuromotor functioning and parental anxiety is scarce. Differences between mothers and fathers may exist.
Objective:
We aimed to compare anxiety levels in parents of extremely preterm infants with those of working adults throughout the first two years after NICU discharge, and to investigate the differences between mothers and fathers. Secondly, we aimed to examine associations between neuromotor functioning, perinatal risk factors and parental anxiety.
Design/Methods:
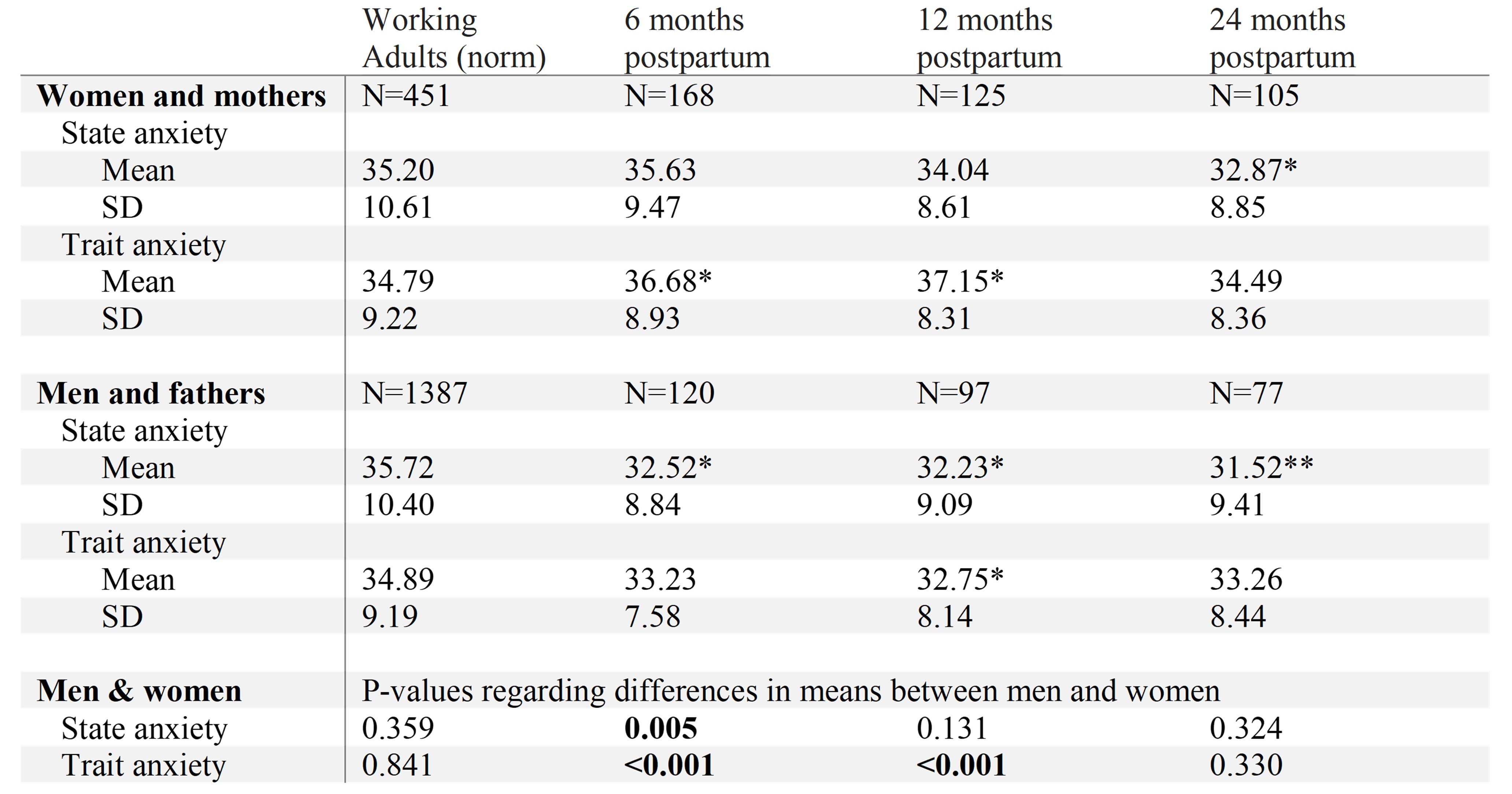
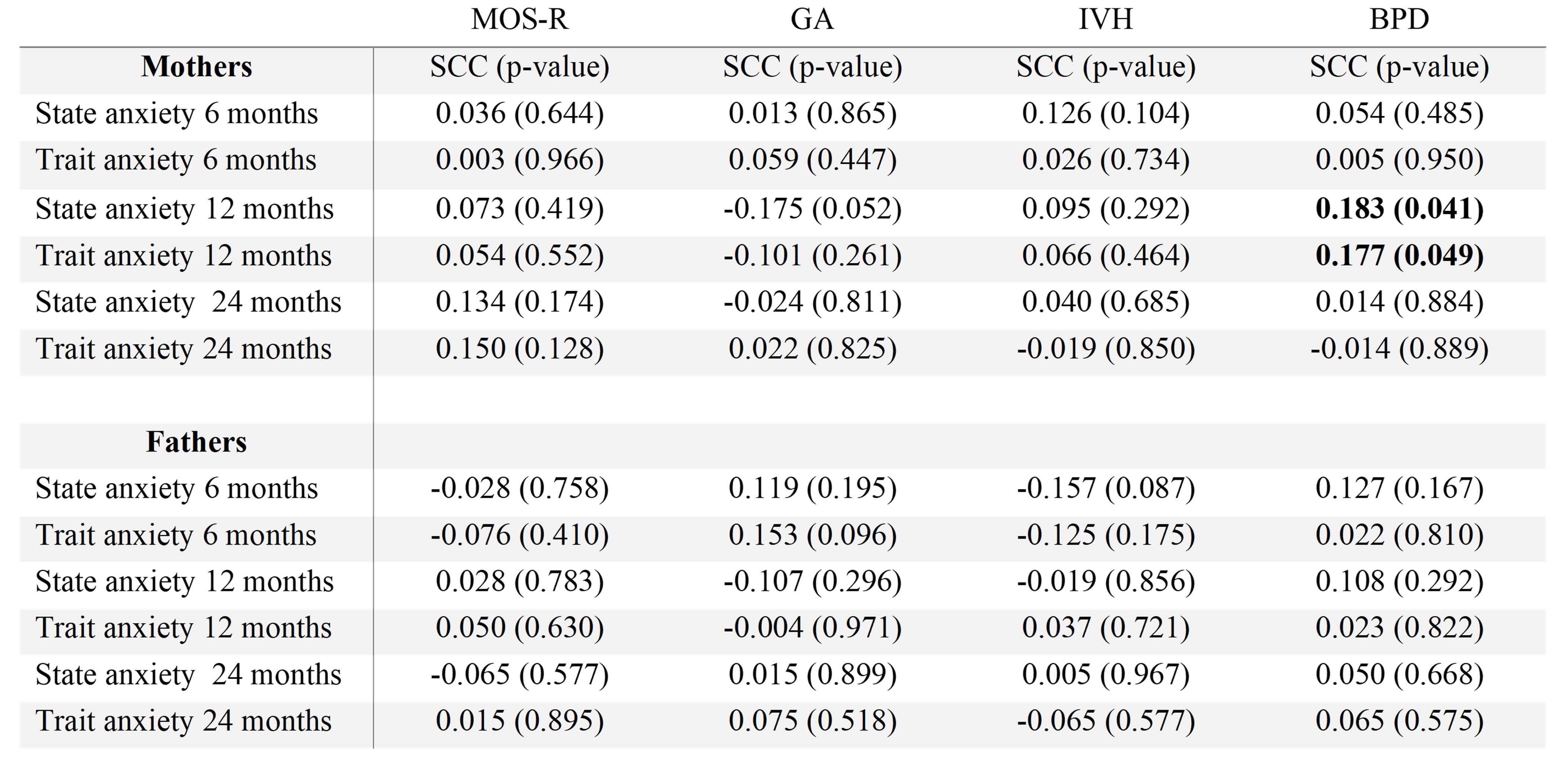
From a cohort of 280 extremely preterm infants (GA < 30wks and BW < 1000g) born between 2015 and 2022, 189 parents completed the State-Trait Anxiety Inventory (STAI) at 6, 12 and/or 24 months. STAI-scores consist of two sets of 20 statements evaluating how respondents feel ‘right now’ (State) and how people ‘generally feel’ (Trait). Neuromotor functioning was assessed using spontaneous movement quality and associated motor optimality score revised (MOS-R) at 3 months corrected age. Perinatal risk factors included GA, intraventricular hemorrhage (IVH) and bronchopulmonary dysplasia (BPD). A series of variance analyses, paired samples t-tests, and bivariate correlations were used to evaluate the study aims.
Results:
Mothers and fathers did not report elevated levels of state anxiety, and the scores decreased over time. Trait anxiety was only elevated in mothers at 6 and 12 months (Table 1). Mothers had higher state anxiety at 6 months and trait anxiety at 6 and 12 months than fathers (p=0.005, p< 0.001, and p< 0.001, respectively). Parental anxiety levels did not associate with MOS-R, GA or IVH. State and Trait scores of mothers at 12 months were significantly associated with BPD (Table 2, r=0.183, p=0.041 and r=0.177, p=0.049).
Conclusion(s):
Anxiety levels of mothers and fathers after NICU discharge are generally comparable to those of working adults. State anxiety decreased between 6 and 24 months, indicating increased confidence. Only at 6 months, maternal state anxiety was higher than paternal state anxiety. Parental anxiety was not primarily associated with infant neuromotor development or perinatal risk factors, except for higher levels of maternal anxiety of infants with BPD at 12 months. It can be considered reassuring that the majority of parents did not experience increased levels of anxiety throughout the two years after NICU discharge.