Neonatal Pulmonology
Neonatal Pulmonology 2: BPD Clinical
258 - Association of Z-scores for Growth with Time to Discontinuation of Positive Airway Pressure in Infants with Grade 2/3 BPD
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 258
Publication Number: 258.34
Publication Number: 258.34
Michelle V. Pfeffer, Nationwide Children's Hospital, Columbus, OH, United States; Carl Backes, Nationwide Children's Hospital, Columbus, OH, United States; Matthew Kielt, Nationwide Children's Hospital, Columbus, OH, United States; Audrey Miller, Nationwide Children's Hospital, Columnus, OH, United States
- MP
Michelle V. Pfeffer, MD (she/her/hers)
Resident
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background: Approximately 46% of infants with bronchopulmonary dysplasia (BPD) receive protracted treatment with non-invasive (grade 2) or invasive (grade 3) positive airway pressure (PAP) at 36 weeks’ post-menstrual age (PMA). Among infants with grade 2/3 BPD, the time required to discontinue PAP is highly variable and there are no evidence-based strategies that facilitate earlier discontinuation from PAP. Adequate growth is important for pulmonary development and function; however, whether z-scores for growth are associated with time to discontinuation of PAP in infants with grade 2/3 BPD remains unknown.
Objective: To estimate the association between higher z-scores for weight and length, measured at 36 weeks’ PMA, with earlier time to discontinuation of PAP in infants with grade 2/3 BPD.
Design/Methods: We performed a retrospective cohort study of infants born < 32 weeks’ gestation and admitted to our referral BPD center between January 2010 and September 2022. Infants admitted prior to 36 weeks’ PMA with a diagnosis of grade 2/3 BPD by 2019 Neonatal Research Network criteria were included. Infants with genetic syndromes or congenital heart defects were excluded. Z-scores for weight and length at 36 weeks’ PMA were calculated using Fenton growth charts. Cox proportional hazard models were used to estimate the association between z-scores for weight and length at 36 weeks’ PMA, respectively, with time (in days after 36 weeks’ PMA) to discontinuation of PAP. Multivariable models were adjusted for gestational age, small-for-gestational age (SGA) status at birth, and BPD grade.
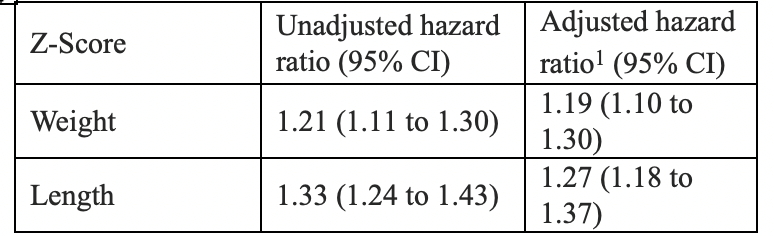
Results: Among 646 included infants, 464 (72%) were diagnosed with grade 2 BPD and 182 (28%) were diagnosed with grade 3 BPD. Cohort subjects were born extremely preterm, with extremely low birth weights, and were predominantly male (Table 1). Fifteen (2%) subjects died prior to hospital discharge. Median z-scores for weight and length at 36 weeks’ PMA were -1.52 (IQR –2.24 to –0.91) and –2.39 (IQR -3.19 to –1.79), respectively. Hazard ratios (HR) adjusted for gestational age, SGA, and BPD grade, demonstrated a significant association between z-scores for weight (HR 1.19, 95% CI 1.10 to 1.30) and length (HR 1.27, 95% CI 1.18 to 1.37) at 36 weeks’ PMA, respectively, with time to discontinuation of PAP. (Table 2)
Conclusion(s): Higher z-scores for weight and length at 36 weeks’ PMA were associated with an earlier time to discontinuation of PAP respiratory support in a cohort of infants with grade 2/3 BPD. Further studies are needed to validate the association of growth with pulmonary function in infants with BPD.
.png)