Back
Background: Bronchopulmonary dysplasia (BPD) contributed to one of major burdens in neonatal care. Early recognition of the high-risk population is crucial for clinical decision-making. Jensen in 2019 developed a new definition of BPD based on evidence to predict early childhood morbidity. The association between early accumulations of oxygen therapy, the ventilator support mean airway pressure (MAP) and the severity of BPD based on new definition is unknown.
Objective: We aim to the impact of the accumulation of oxygen and MAP within postnatal 14 days on the mortality rate and severity of BPD by the Jensen 2019 definition.
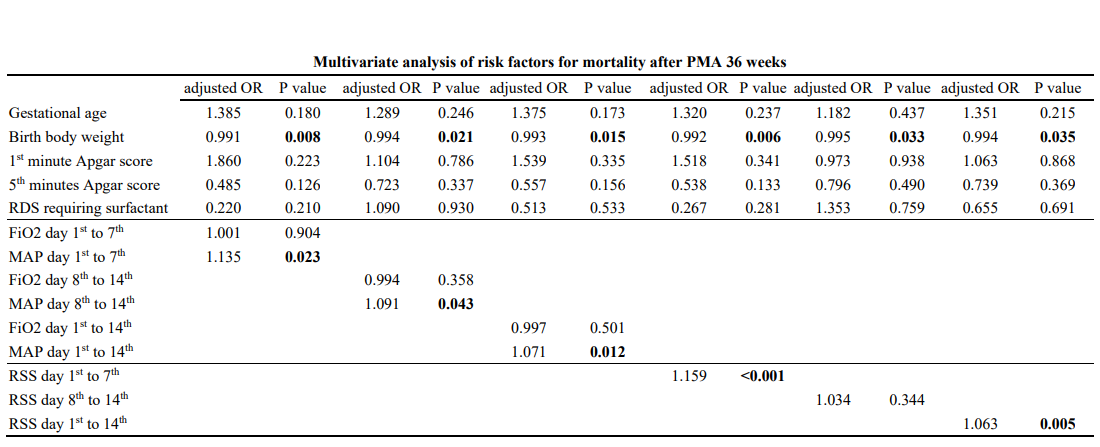
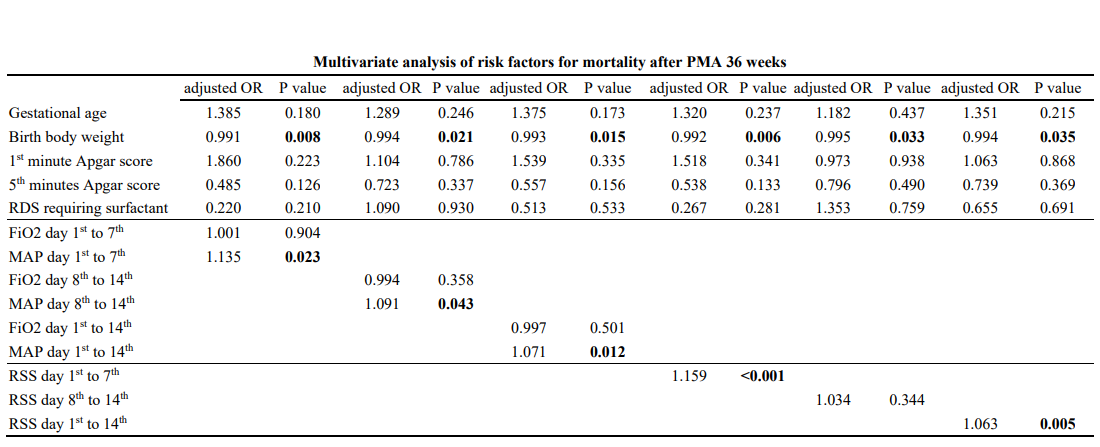
Design/Methods: This is a single-center, retrospective cohort study with data collected from National Cheng Kung University Hospital. From January 2017 to December 2020, infants born < 32 weeks of gestation and birth body weight < 1500g admitted to our neonatal intensive care unit (NICU) were enrolled. We calculated the accumulation of the area under curve (AUC) of FiO2, MAP and the respiratory severity score (RSS) of each infant within 14 days after birth. The risk factors included gestational age, birth body weight, gender, delivery route, Apgar score at the first and fifth minutes, respiratory distress syndrome (RDS) requiring surfactant, necrotizing enterocolitis (NEC) and patent ductus arteriosus (PDA) with treatment. Logistic regression was used to identify the risk factors and the accumulation of the AUC of FiO2, MAP, RSS in different postnatal periods (within the 1stto 7th days, the 8th to 14th days and the 1st to 14th days after birth) associated with the mortality after postmenstrual age (PMA) 36 weeks. Multinomial model was used to identify the association between the accumulation of the AUC of FiO2, MAP, RSS in different postnatal periods and the severity of BPD based on the Jensen’s definition.
Results: A total of 247 infants were enrolled. Based on Jensen’s definition, 2.4% infants were stage I, 44.5% infants were stage II,4.1% infant were stage III. And 49% infants had no BPD. The accumulated MAP within first week (aOR=1.135, P=0.023), the second week (aOR=1.091, P=0.043), 14 days (aOR=1.071, P=0.012) of life were significantly associated with mortality after PMA 36 week. The accumulated FiO2 within the first week, in the second week, in the 14 days and the accumulated RSS within second weeks and within 14 days of life have good discrimination of severity of BPD.
Conclusion(s): The need of respiratory ventilatory support and FiO2 within 14 days after birth were associated with the mortality after PMA 36 weeks and the severity of BPD by Jensen’s definition.
.png)
.png)
Neonatal Pulmonology
Neonatal Pulmonology 3: BPD Clinical and Translational
273 - The association between early respiratory ventilatory support and mortality, severity of bronchopulmonary dysplasia in very low birth weight preterm infants
Sunday, April 30, 2023
3:30 PM – 6:00 PM ET
Poster Number: 273
Publication Number: 273.341
Publication Number: 273.341
Yi Han Su, National Cheng Kung University Hospital, tainan, Tainan, Taiwan (Republic of China); Yen Ju Chen, National Cheng Kung University hospital, Tainan, Tainan, Taiwan (Republic of China); Ts-Ting Wang, Ditmanson Medical Foundation Chia-Yi Christian Hospital, Tainan, Tainan, Taiwan (Republic of China); Yun-Hsiang Yang, NCKUH, Tainan, Tainan, Taiwan (Republic of China); Wei-Ting Lin, National Cheng Kung University Hospital, Tainan City CentralWest distinction, Tainan, Taiwan (Republic of China); WEIYING CHU, National Cheng Kung University Hospital, Tainan, Tainan, Taiwan (Republic of China); Yu-Shan Chang, National Cheng Kung University Hospital, Tainan, Tainan, Taiwan (Republic of China); Yung-Chieh Lin, National Cheng Kung University & Hospital, Tainan, Tainan, Taiwan (Republic of China); Chyi-Her Lin, E-Da Hospital, Kaohsiung, Kaohsiung, Taiwan (Republic of China); Yuh-Jyh Lin, National Cheng-Kung U Hospital, Tainan, Tainan, Taiwan (Republic of China)
- YS
Yi Han Su
fellow
National Cheng Kung University Hospital
tainan, Tainan, Taiwan (Republic of China)
Presenting Author(s)
Background: Bronchopulmonary dysplasia (BPD) contributed to one of major burdens in neonatal care. Early recognition of the high-risk population is crucial for clinical decision-making. Jensen in 2019 developed a new definition of BPD based on evidence to predict early childhood morbidity. The association between early accumulations of oxygen therapy, the ventilator support mean airway pressure (MAP) and the severity of BPD based on new definition is unknown.
Objective: We aim to the impact of the accumulation of oxygen and MAP within postnatal 14 days on the mortality rate and severity of BPD by the Jensen 2019 definition.
Design/Methods: This is a single-center, retrospective cohort study with data collected from National Cheng Kung University Hospital. From January 2017 to December 2020, infants born < 32 weeks of gestation and birth body weight < 1500g admitted to our neonatal intensive care unit (NICU) were enrolled. We calculated the accumulation of the area under curve (AUC) of FiO2, MAP and the respiratory severity score (RSS) of each infant within 14 days after birth. The risk factors included gestational age, birth body weight, gender, delivery route, Apgar score at the first and fifth minutes, respiratory distress syndrome (RDS) requiring surfactant, necrotizing enterocolitis (NEC) and patent ductus arteriosus (PDA) with treatment. Logistic regression was used to identify the risk factors and the accumulation of the AUC of FiO2, MAP, RSS in different postnatal periods (within the 1stto 7th days, the 8th to 14th days and the 1st to 14th days after birth) associated with the mortality after postmenstrual age (PMA) 36 weeks. Multinomial model was used to identify the association between the accumulation of the AUC of FiO2, MAP, RSS in different postnatal periods and the severity of BPD based on the Jensen’s definition.
Results: A total of 247 infants were enrolled. Based on Jensen’s definition, 2.4% infants were stage I, 44.5% infants were stage II,4.1% infant were stage III. And 49% infants had no BPD. The accumulated MAP within first week (aOR=1.135, P=0.023), the second week (aOR=1.091, P=0.043), 14 days (aOR=1.071, P=0.012) of life were significantly associated with mortality after PMA 36 week. The accumulated FiO2 within the first week, in the second week, in the 14 days and the accumulated RSS within second weeks and within 14 days of life have good discrimination of severity of BPD.
Conclusion(s): The need of respiratory ventilatory support and FiO2 within 14 days after birth were associated with the mortality after PMA 36 weeks and the severity of BPD by Jensen’s definition.
.png)
.png)
