Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 3: Physiology 2 and Clinical Outcomes
344 - Spontaneous Intestinal Perforations (SIP) in Extreme Preterm Infants before, during and after a period of Prophylactic Hydrocortisone Treatment – Experience from a UK Level III Neonatal Unit
Publication Number: 344.346
- CR
Charles C. Roehr, MD, PhD. (he/him/his)
Professor of Neonatology and Perinatal Research
University of Bristol
Bristol, England, United Kingdom
Presenting Author(s)
Background:
Bronchopulmonary dysplasia (BPD) is a serious complication of extreme premature birth. Strategies to prevent BPD include targeted treatment with postnatal corticosteroids. Significant adverse effects of corticosteroid treatment include poorer neuro-developmental outcome and spontaneous intestinal perforation (SIP). Clinical trials of prophylactic hydrocortisone (HC) to counter transient functional adrenal insufficiency (TFAI), conducted in preterm infants of predominantly higher gestational ages, showed improving BPD and survival rates without other significant adverse effects.
In November 2020, our tertiary neonatal unit, which specialises in the care of the most premature infants (MPI, defined as 22 - 25 completed weeks’ gestation) joined a regional quality improvement program. The program promotes a bundle of perinatal interventions to improve survival and reduce brain injury of babies born prematurely. It includes early prophylactic HC for infants < 28 weeks’ gestation. Five months into the program, we observed increased rates of SIP in MPI at our centre. We hypothesised that protocolised early prophylactic early HC contributed to the increase of SIP in MPI.
Objective: To present data on the incidence of SIP in MIP during three time periods of HC use.
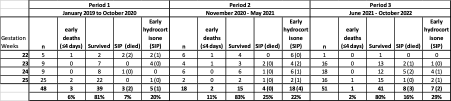
Design/Methods: Prospective, observational single centre study of early HC treatment in MPI. Three time periods are defined, 1) targeted use of HC following biochemical evidence of TFAI, 2) period of protocolised prophylactic HC for all preterms < 28 weeks, and 3) post-prophylactic period, with targeted HC treatment for TFAI. Descriptive statistics with Microsoft Excel.
Results:
From January 2019 - October 2022, 117 MPI were treated (table 1). Excluding early deaths (≤4 days of age) in period 1, three of 45 MPI suffered SIP (incidence 7%), of which one had received HC; in period 2, all 16 infants were treated with prophylactic HC, four developed SIP (incidence 25%); in period 3, eight of 50 treated infants suffered SIP (incidence 16%), of whom 2 received HC for TFAI. The incidence of SIP in those receiving early HC was similar in 3 periods (20%, 22% and 29% respectively).
Conclusion(s): In MIP, early HC was associated with an increased risk of SIP. The peak incidence of SIP was during a period of protocolised prophylactic HC use. Acknowledging the potential benefits of early HC treatment but also the potential for harm, together with the lack of data on safety and efficacy for MPI from the primary trials, it seems worth considering a separate randomised controlled trial on early HC in infants born < 26 weeks’ gestation.