Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 2: Physiology 1
327 - Chorioamnionitis-induced fetal breathing movement inhibition is not restored by Ibuprofen.
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 327
Publication Number: 327.345
Publication Number: 327.345
Robert Galinsky, Hudson Institute of Medical Research, MELBOURNE, Victoria, Australia; Nhi T. Tran, The Hudson Institute of Medical Research, Melbourne, Victoria, Australia; Sharmony B. Kelly, The Hudson Institute/Monash University, Melbourne, Victoria, Australia; Graeme Polglase, Hudson Institute of Medical Research, Melbourne, Victoria, Australia

Graeme Polglase, PhD (he/him/his)
Associate DIrector
Hudson Institute of Medical Research
Melbourne, Victoria, Australia
Presenting Author(s)
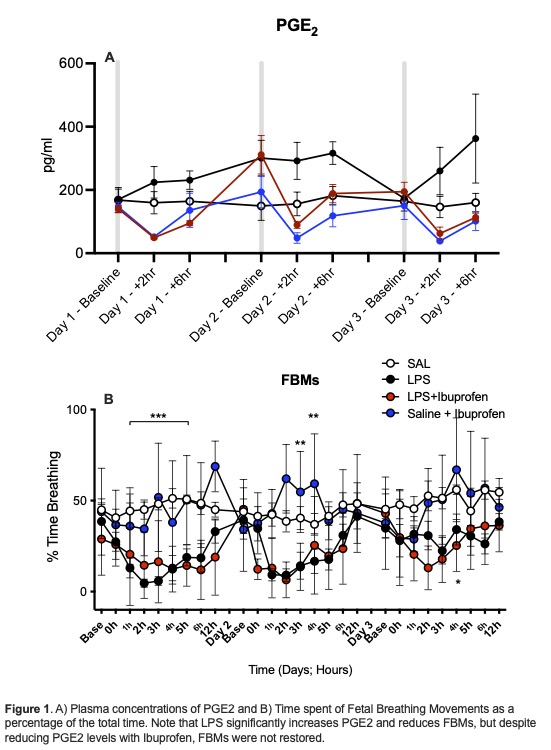
Background: Preterm infants exposed to chorioamnionitis during pregnancy are at increased risk of apnoea after birth. We have previously shown in late preterm fetal sheep that lipopolysaccharide (LPS) exposure inhibits fetal breathing movements (FBM) and was associated with increased prostaglandin E2 (PGE2) within plasma and the brainstem respiratory centres.
Objective: We hypothesised that inhibiting increases of PGE2 with Ibuprofen, a non-steroidal PGE2 inhibitor, would prevent FBM inhibition.
Design/Methods: Fetal sheep (~125 days gestation (dGA)) were sterilely instrumented with tracheal, arterial and venous catheters to measure FBM, heart rate, blood pressure, blood gases and administer interventions. At ~130 dGA, fetuses received saline or escalating doses of LPS (300ng, 600ng, 1.2ug i.v.) over 3 days, with each LPS event followed by saline or 5mg/kg/d ibuprofen. FBMs were assessed using LabChart. PGE2 expression in brainstem respiratory centres was assessed by immunohistochemistry. PGE2 levels in cerebrospinal fluid (CSF) and plasma were assessed by ELISA.
Results: LPS significantly increased plasma PGE2 levels and transiently inhibited FBMs. This coincided with a significant increase in PaCO2 and reduction in PaO2.
Ibuprofen treatment following LPS administration significantly reduced circulating PGE2 levels and PGE2 levels in the brainstem respiratory centre (RTN/pFRG and Raphe nuclei) but not in the CSF and pre-BötC and Hypoglossal nucleus (XII). Despite the reductions in PGE2, Ibuprofen treatment did not restore fetal breathing movement inhibition induced by LPS.
Conclusion(s): Our data suggests FBM inhibition is not exclusively driven by high PGE2 levels, challenging our current understanding. Further investigation elucidating the mechanisms and pathways underlying respiratory depression following chorioamnionitis in preterm newborns are needed to develop treatment strategies.