Neonatal Follow-up
NICU Follow Up and Neurodevelopment 5: Impact of Parents and Social Determinants of Health
152 - Wellbeing and Posttraumatic Growth in Birthing Parents After Preterm Birth
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 152
Publication Number: 152.363
Publication Number: 152.363
Isobel Newton-Bennett, University of Tasmania, Rokeby, Tasmania, Australia; Carmina Erdei, Harvard Medical School, Boston, MA, United States; Grace C. Fitzallen, University of Tasmania, South Launceston, Tasmania, Australia
- GF
Grace C. Fitzallen, PhD (she/her/hers)
University of Tasmania
South Launceston, Tasmania, Australia
Presenting Author(s)
Background: There is extensive knowledge of maternal psychopathology after preterm birth. However, there is limited understanding of related, but distinct constructs of wellbeing and posttraumatic growth, and their associated protective factors.
Objective: To describe wellbeing and posttraumatic growth in birthing parents of children born preterm (< 37 weeks of gestation) across infancy-toddlerhood (0-2 years), early childhood (3-5 years), and middle childhood (6-9 years); and to identify child and sociodemographic factors associated with greater wellbeing and posttraumatic growth.
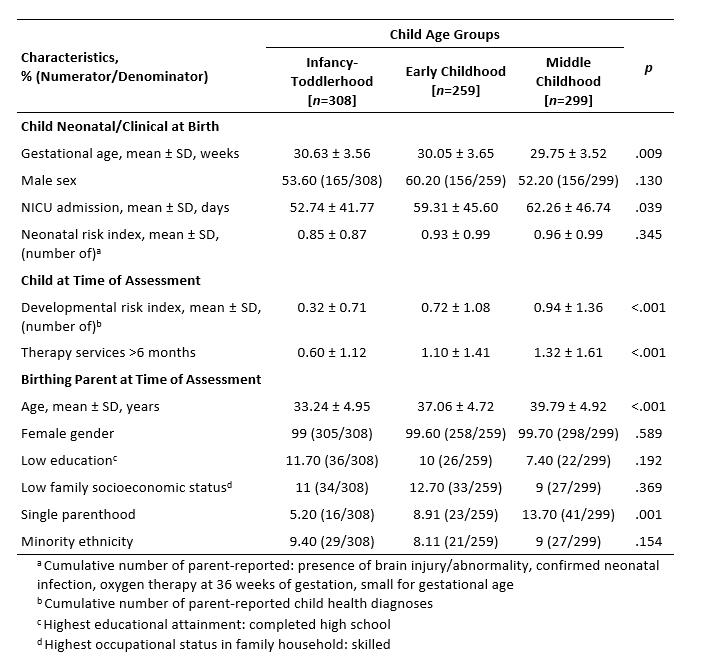
Design/Methods: The sample comprised 866 birthing parents of children born preterm stratified into child age groups (infancy-toddlerhood, n=308; early childhood, n=259; middle childhood, n=299). Sample characteristics are shown in Table 1. Self-reports were collected at a single time-point on the standardized Psychological Wellbeing Scale and Posttraumatic Growth Inventory.
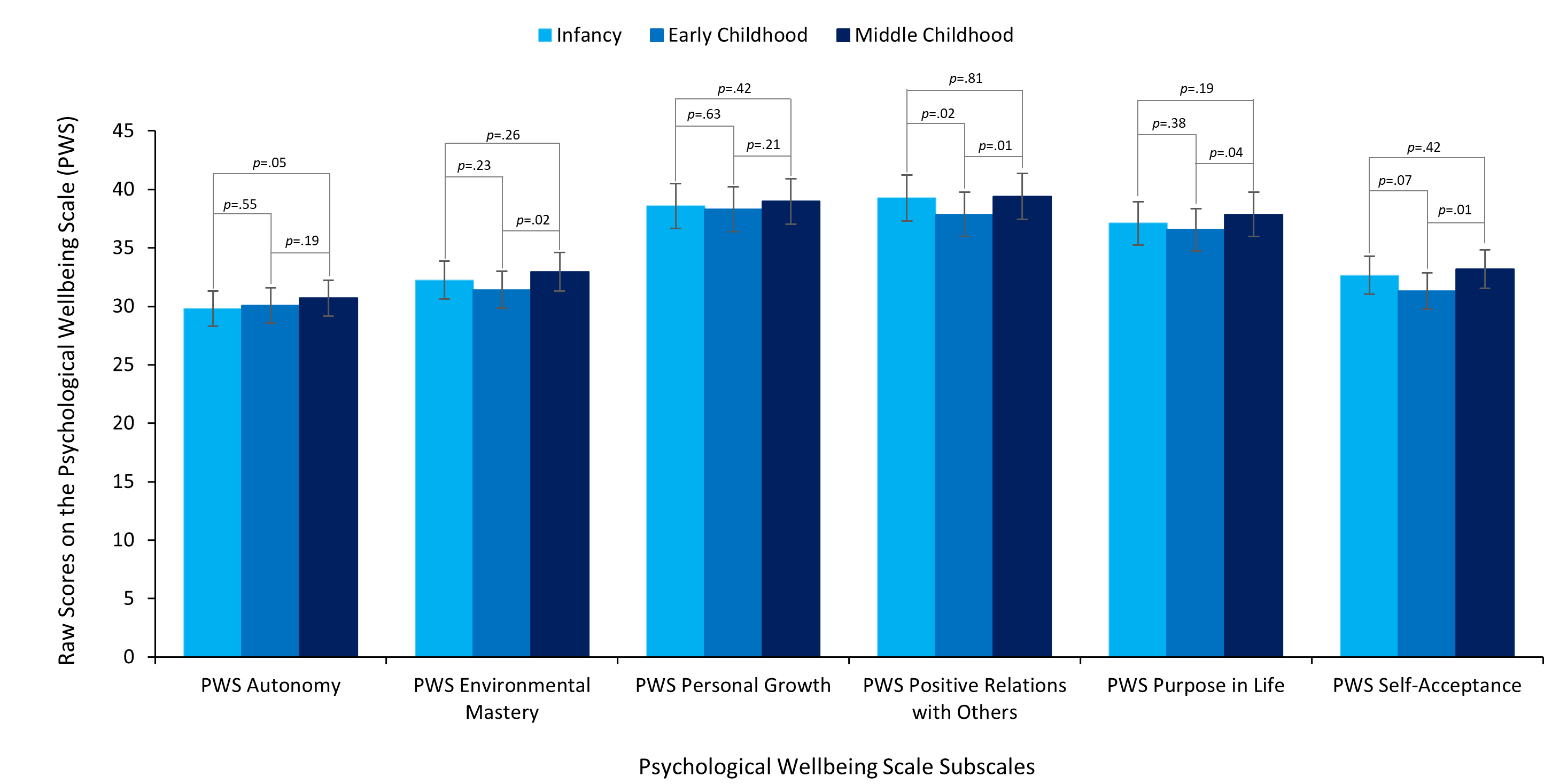
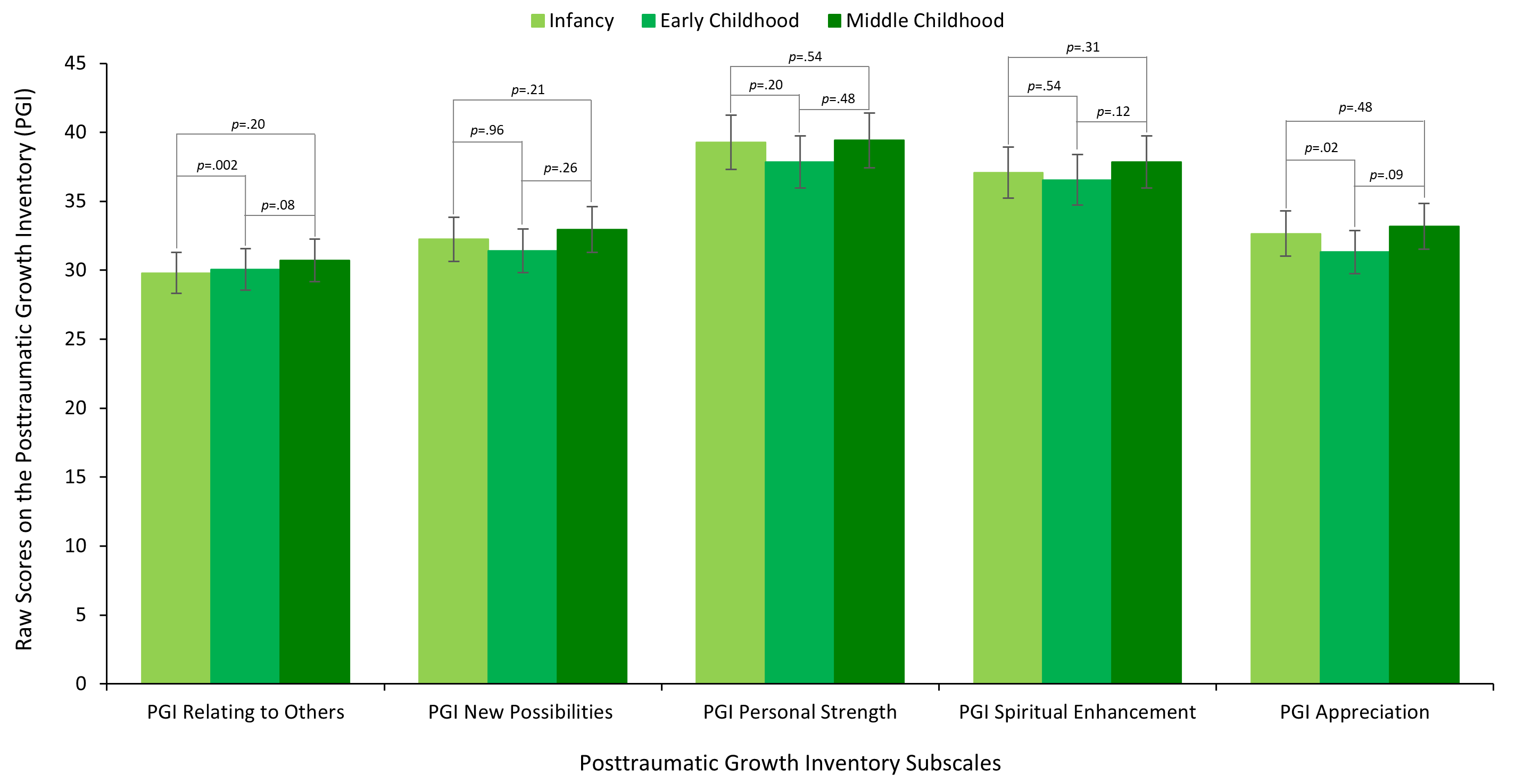
Results: Wellbeing and posttraumatic growth were positively associated (p< .001). Parents of children in middle childhood reported greater scores (p< .05) than early childhood for total wellbeing, environmental mastery (i.e., competence and optimization of the external environment), positive relations with others, purpose in life, and self-acceptance (Figure 1). Parents of infant-toddlers reported greater scores (p< .05) than early childhood for subscales of realting to others and appreciation (Figure 2). Greater wellbeing was associated with earlier gestational age (β=-.116, p=.028), < 50 NICU days (β=-.119, p=.025), lower developmental risk (β=-.176, p< .001), older age at birth (β=.088, p=.03), and higher socioeconomic status (β=-.195, p< .001). Greater posttraumatic growth was associated with higher neonatal risk (β=.156, p< .001), >50 NICU days (β=.130, p=.002), more therapy services (β=.109, p=.005), younger at birth (β=-.153, p< .001), and majority ethnicity (β=-.080, p=.025). Variables explained 8.5% and 10.2%, respectively.
Conclusion(s): Findings demonstrate age-related differences in wellbeing and posttraumatic growth. While wellbeing and posttraumatic growth were related, they were differentially impacted by protective factors spanning neonatal, child concurrent, and sociodemographic factors. Although replication using longitudinal design is recommended, findings highlight the need for more comprehensive and long-term psychological surveillance and targeted support for birthing parents. Research in this area can inform modifiable factors targetable through psychosocial intervention, allowing for optimization of outcomes after preterm birth.