Neonatal Neurology: Clinical Research
Neonatal Neurology 4: Clinical 4
93 - Altered trajectory of the incidence of brush as determined via preterm electroencephalogram is associated with brain maturation or injury
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 93
Publication Number: 93.336
Publication Number: 93.336
Anna Shiraki, Nagoya University Graduate School of Medicine, Nagoya, Aichi, Japan; Hiroyuki Kidokoro, Nagoya University Graduate School of Medicine, Nagoya, Aichi, Japan; Hama Watanabe, Graduate School of Education, The University of Tokyo, Bunkyo-ku, Tokyo, Japan; Gentaro Taga, Graduate School of Education, The University of Tokyo, Bunkyo-ku, Tokyo, Japan; Tsu Yoshimura, Nagoya University Graduate School of Medicine, Nagoya, Aichi, Japan; Hajime Narita, Nagoya Univercity Graduate School of Medicine, Nagoya, Aichi, Japan; Takamasa Mitsumatsu, Nagoya University Graduate School of Medicine, nagoya, Aichi, Japan; Sumire Kumai, Nagoya University Graduate School of Medicine, Nagoya, Aichi, Japan; Ryosuke Suzui, Nagoya University Graduate School of Medicine, Nagoya, Aichi, Japan; Fumi Sawamura, Nagoya University Graduate School of Medicine, Nagoya, Aichi, Japan; Takashi Maeda, Nagoya university hospital, nagoya, Aichi, Japan; Yuji Ito, Nagoya University, Nagoya, Aichi, Japan; Hiroyuki Yamamoto, Nagoya University Graduate School of Medicine, Nagoya, Aichi, Japan; Tomohiko Nakata, Nagoya University Graduate School of Medicine, Nagoya, Aichi, Japan; Yoshiaki Sato, Nagoya University Hospital, Nagoya, Aichi, Japan; Masahiro Hayakawa, Nagoya University Hospital, Miyoshi, Aichi, Japan; Jun Natsume, Nagoya University Graduate School of Medicine, Nagoya, Aichi, Japan
Anna Shiraki, MD (she/her/hers)
PhD student
Nagoya University Graduate School of Medicine
Nagoya, Aichi, Japan
Presenting Author(s)
Background: “Brush” is a characteristic fast activity pattern in a preterm electroencephalogram (EEG) that changes in incidence during development. However, its clinical significance has not been established.
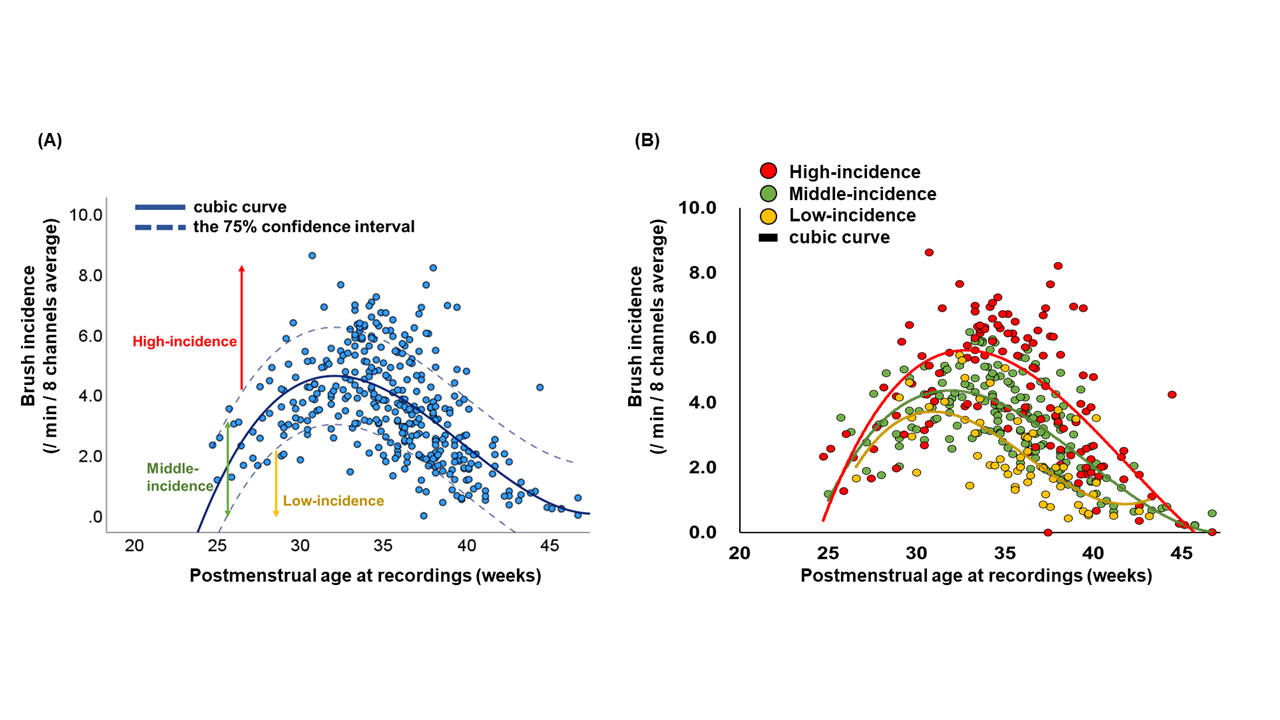
Objective: We quantitatively clarified the trajectory of brush incidence between 24 and 46 weeks postmenstrual age (PMA) and explored whether different trajectories are associated with brain immaturity or injury in preterm infants.
Design/Methods: In all, 365 EEG from 100 preterm infants were collected from the preterm cohort in our hospital. EEG was recorded with at least eight electrodes. We utilized an automated detection algorithm for brushes in the bi-polar EEG envelope after filtering at 8–25 Hz with a duration of 0.3–1.2 s and an average amplitude > 10 µV within a 0.3 s sliding window. Brush incidence was calculated as an 8-channel average per minute. All EEG records were reviewed and classified into normal, mild dysmature (2 weeks immature relative to an infant’s PMA), and severe dysmature (3 weeks or more immature). White matter injury (WMI) was evaluated by magnetic resonance imaging (MRI) at the term-equivalent age and classified into normal, mild (punctate lesions), and severe (cystic lesions). Based on brush incidence, infants were classified into low-, middle-, and high-incidence groups using 75% confidential intervals. The Fisher-Freeman-Halton exact test was used to examine the associations between the high- and low-incidence groups and EEG/MRI factors.
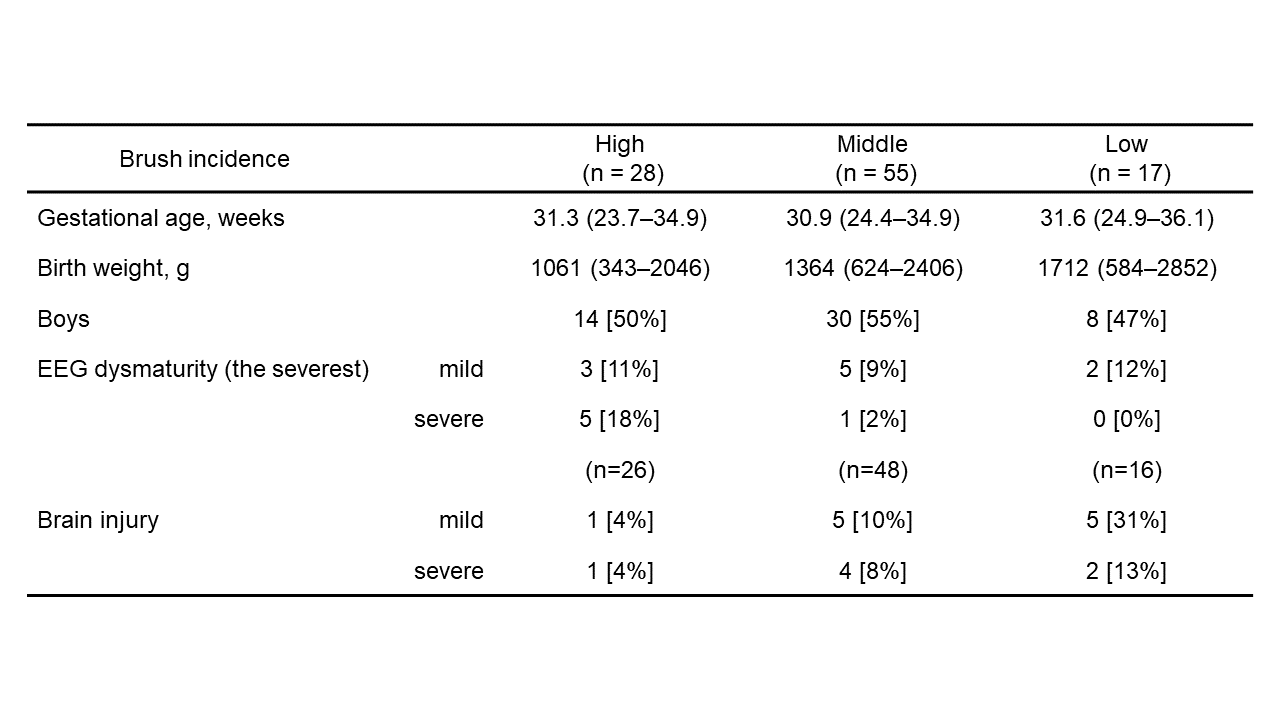
Results: The infants’ characteristics are shown in Table 1. The gestational ages at birth and recording were 23.7–36.1 and 24.7–46.7 weeks, respectively. Brush incidence peaked at 32–34 weeks PMA and decreased gradually toward 46 weeks PMA (Figure 1). The high-incidence group contained more infants with a severe dysmature pattern (p = 0.010) and the low-incidence group contained more infants with mild WMI (p = 0.015) than the others. In contrast, the high-incidence group and the WMIs and the low-incidence group and EEG maturation were not associated. These results were elaborated by the trajectories of brush incidence separated by the different EEG maturation or WMI groups. Infants with a severe dysmature pattern had a delayed decrease at 34–40 weeks than those with normal maturation according to EEG. Infants with mild WMI had fewer brushes than those without WMI (Figure 2).
Conclusion(s): Our data demonstrate the developmental trajectory of brush incidence between 24 and 46 weeks PMA in preterm infants using an automated detection algorithm. The different trajectories are useful neurodevelopmental markers for preterm infants.
.png)
