Back
Background: Disruption of lung development from antenatal stress, including inflammation with chorioamnionitis (CA), is associated with placental dysfunction and high risk of developing bronchopulmonary dysplasia (BPD) and pulmonary hypertension (PH) after preterm birth. Although antenatal steroids (ANS) improve many outcomes in preterms, ANS therapy has not been shown to reduce the risk for BPD or PH. Further the effects of ANS on placental function are unknown.
Objective: We hypothesize that maternal betamethasone (BM) therapy preserves lung development and prevents PH in experimental CA and that these effects are associated with steroid-targeting of placental signaling to optimize the intrauterine environment.
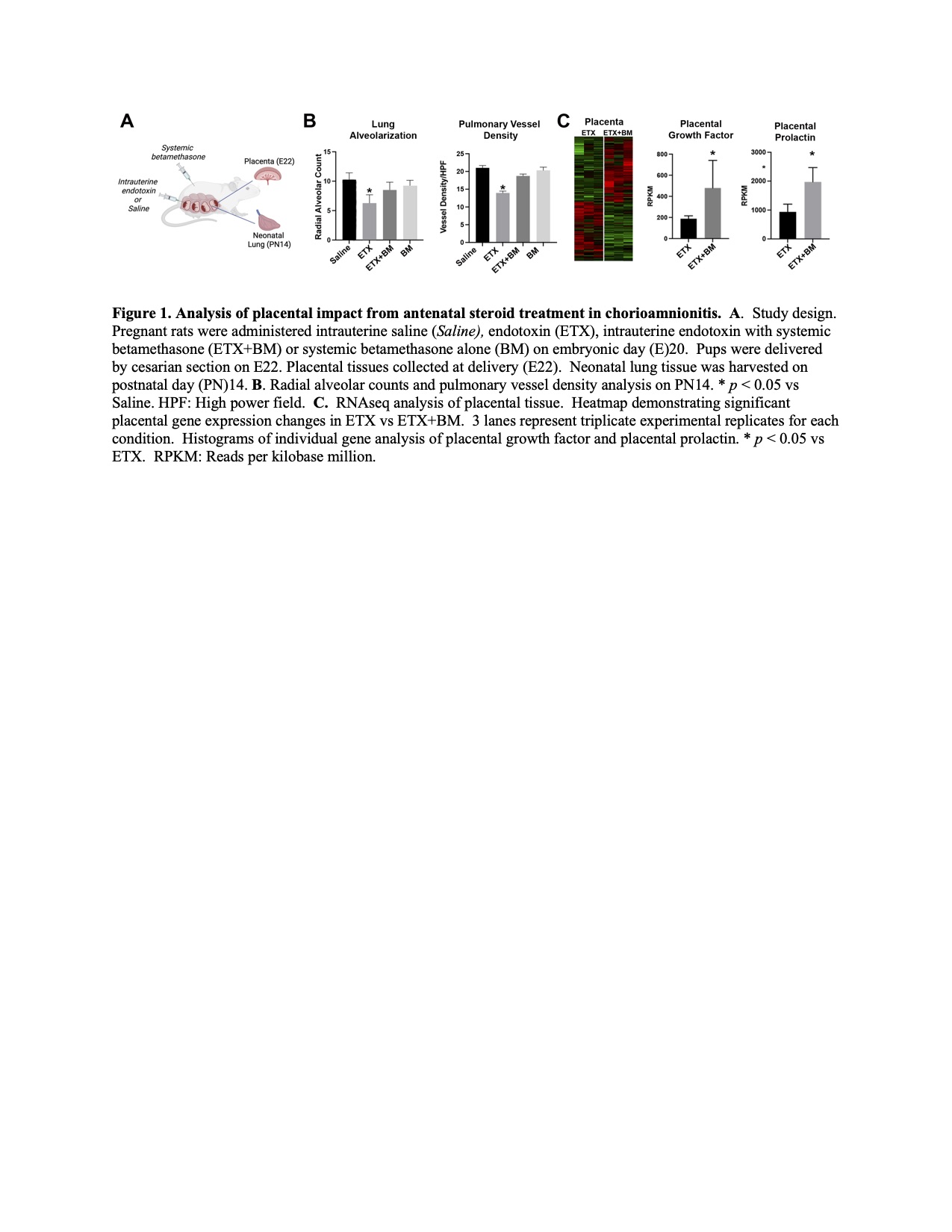
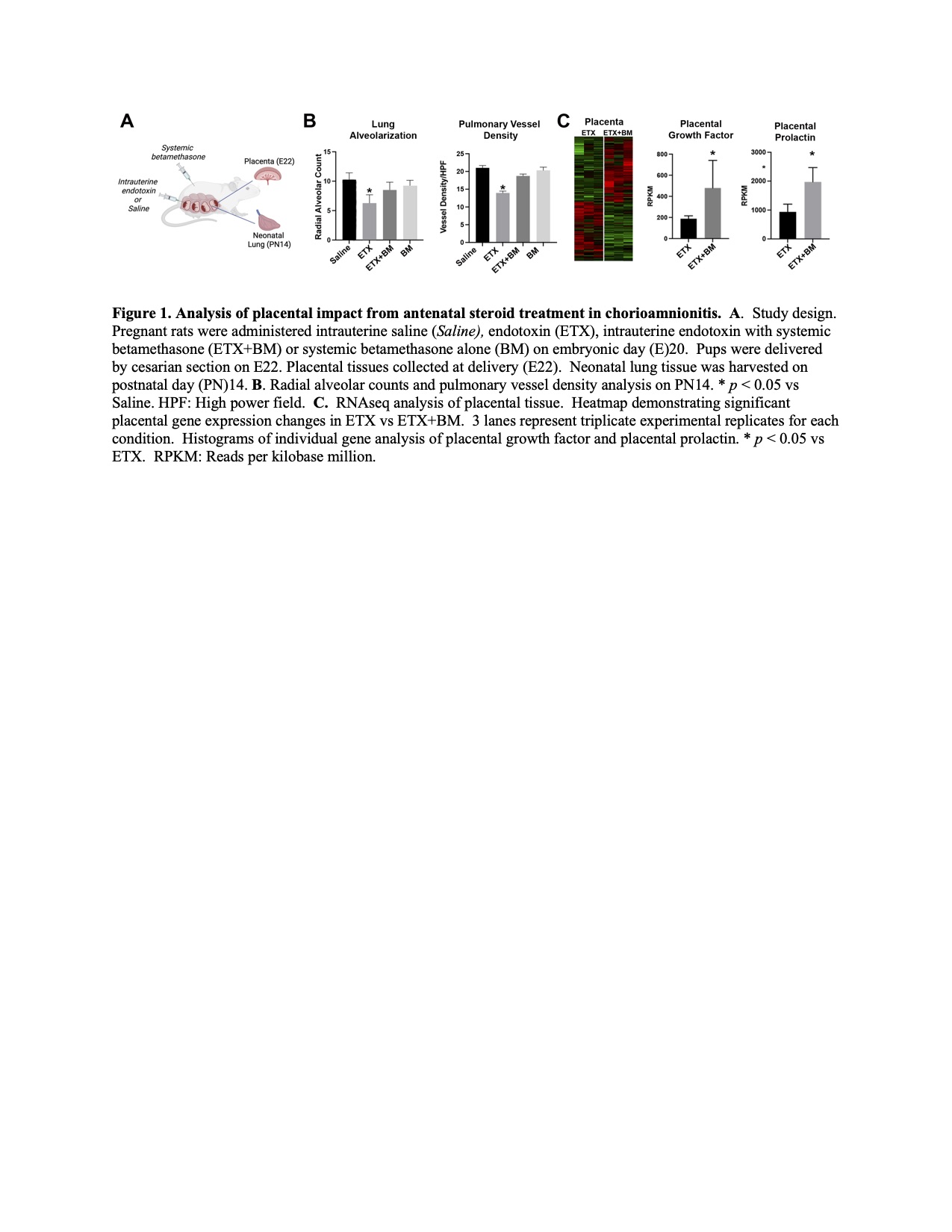
Design/Methods: To investigate placental-specific mechanisms through which fetal lung development can be preserved after exposure to injury due to intrauterine inflammation, we created a model of CA and studied the effects of antenatal steroid administration. Pregnant dams were administered either saline, intra-amniotic endotoxin (IA ETX), ETX plus systemic BM (ETX+BM) or systemic BM alone (BM) on embryonic day (E)20. We collected placental tissues at delivery (E22) and performed structural and functional analysis of infant lungs on postnatal day (PN)14 (Fig. 1A).
Results: In comparison with controls, IA ETX impaired lung growth, increased total respiratory resistance, reduced lung compliance, and increased right ventricle hypertrophy (RVH) at PN14. Maternal BM treatment of ETX-exposed fetal rats preserved lung structure and function and prevented RVH. BM treatment reduced total lung resistance by 15.3% and improved compliance by 9.5% (p< 0.05 for each parameter). BM preserved lung alveolarization as measured by radial alveolar counts (RAC; (p< 0.05), increased pulmonary vessel density (p< 0.05), and improved RVH by 42% (p< 0.05) (Fig 1B). RNAseq analysis of placental tissue identified over 330 genes with significantly altered expression patterns between ETX vs ETX+BM pregnancies. Pathway enrichment analysis of placental-specific secreted factors identified a striking upregulation of the pro-angiogenic genes, placental growth factor (PGF; 2.1fold increase, p < 0.05) and placental prolactin (PRL; 2.5 fold increase, p < 0.05) (Fig. 1C).
Conclusion(s): Maternal BM treatment preserved lung development and prevented PH in a model of BPD induced by CA, and maternal BM enhanced placental PGF and PRL expression after exposure to inflammation. We speculate that ANS enhance placental function through upregulation of PGF and PRL.
Neonatal Pulmonology
Neonatal Pulmonology 1: Lung Development, Control of Breathing
240 - Placental Growth Factor and Prolactin Upregulation Are Associated with Improved Lung Development After Antenatal Betamethasone Treatment in Experimental Chorioamnionitis
Sunday, April 30, 2023
3:30 PM – 6:00 PM ET
Poster Number: 240
Publication Number: 240.339
Publication Number: 240.339
Adom Netsanet, University of Colorado School of Medicine, Aurora, CO, United States; Gregory Seedorf, University of Colorado School of Medicine, Aurora, CO, United States; Steven Abman, University of Colorado School of Medicine, Denver, CO, United States; Elizabeth Taglauer, Boston University School of Medicine, Boston, MA, United States

Adom Netsanet, B.A. (she/her/hers)
Medical Student
University of Colorado School of Medicine
Aurora, Colorado, United States
Presenting Author(s)
Background: Disruption of lung development from antenatal stress, including inflammation with chorioamnionitis (CA), is associated with placental dysfunction and high risk of developing bronchopulmonary dysplasia (BPD) and pulmonary hypertension (PH) after preterm birth. Although antenatal steroids (ANS) improve many outcomes in preterms, ANS therapy has not been shown to reduce the risk for BPD or PH. Further the effects of ANS on placental function are unknown.
Objective: We hypothesize that maternal betamethasone (BM) therapy preserves lung development and prevents PH in experimental CA and that these effects are associated with steroid-targeting of placental signaling to optimize the intrauterine environment.
Design/Methods: To investigate placental-specific mechanisms through which fetal lung development can be preserved after exposure to injury due to intrauterine inflammation, we created a model of CA and studied the effects of antenatal steroid administration. Pregnant dams were administered either saline, intra-amniotic endotoxin (IA ETX), ETX plus systemic BM (ETX+BM) or systemic BM alone (BM) on embryonic day (E)20. We collected placental tissues at delivery (E22) and performed structural and functional analysis of infant lungs on postnatal day (PN)14 (Fig. 1A).
Results: In comparison with controls, IA ETX impaired lung growth, increased total respiratory resistance, reduced lung compliance, and increased right ventricle hypertrophy (RVH) at PN14. Maternal BM treatment of ETX-exposed fetal rats preserved lung structure and function and prevented RVH. BM treatment reduced total lung resistance by 15.3% and improved compliance by 9.5% (p< 0.05 for each parameter). BM preserved lung alveolarization as measured by radial alveolar counts (RAC; (p< 0.05), increased pulmonary vessel density (p< 0.05), and improved RVH by 42% (p< 0.05) (Fig 1B). RNAseq analysis of placental tissue identified over 330 genes with significantly altered expression patterns between ETX vs ETX+BM pregnancies. Pathway enrichment analysis of placental-specific secreted factors identified a striking upregulation of the pro-angiogenic genes, placental growth factor (PGF; 2.1fold increase, p < 0.05) and placental prolactin (PRL; 2.5 fold increase, p < 0.05) (Fig. 1C).
Conclusion(s): Maternal BM treatment preserved lung development and prevented PH in a model of BPD induced by CA, and maternal BM enhanced placental PGF and PRL expression after exposure to inflammation. We speculate that ANS enhance placental function through upregulation of PGF and PRL.