Neonatal Pulmonology
Neonatal Pulmonology 2: BPD Clinical
255 - Duration of Home Oxygen Therapy in Preterm Infants Diagnosed with Bronchopulmonary Dysplasia: Does Compliance Matter
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 255
Publication Number: 255.34
Publication Number: 255.34
Heather White, University of Massachusetts Medical School, Worcester, MA, United States; Katherine R. Edeburn, UMass Medical School, Worcester, MA, United States; Lawrence Rhein, University of Massachusetts Medical School, Waban, MA, United States

Heather White, MPH, PA-S (she/her/hers)
Research Manager
University of Massachusetts Medical School
Worcester, Massachusetts, United States
Presenting Author(s)
Background: Published studies indicate that up to a third of infants diagnosed with bronchopulmonary dysplasia will require supplemental oxygen at time of neonatal discharge. Currently, there is no consensus-based guidelines to manage home oxygen therapy (HOT) in the outpatient setting. The Recorded Home Oximetry trial was the first to evaluate HOT weaning strategies. It found that recorded home oximetry (RHO) between clinic visits shortened duration of HOT, decreased adverse events, and improved growth. Now, the RHO Program is being implemented at 14 centers across the United States (U.S.) as part of a larger implementation trial.
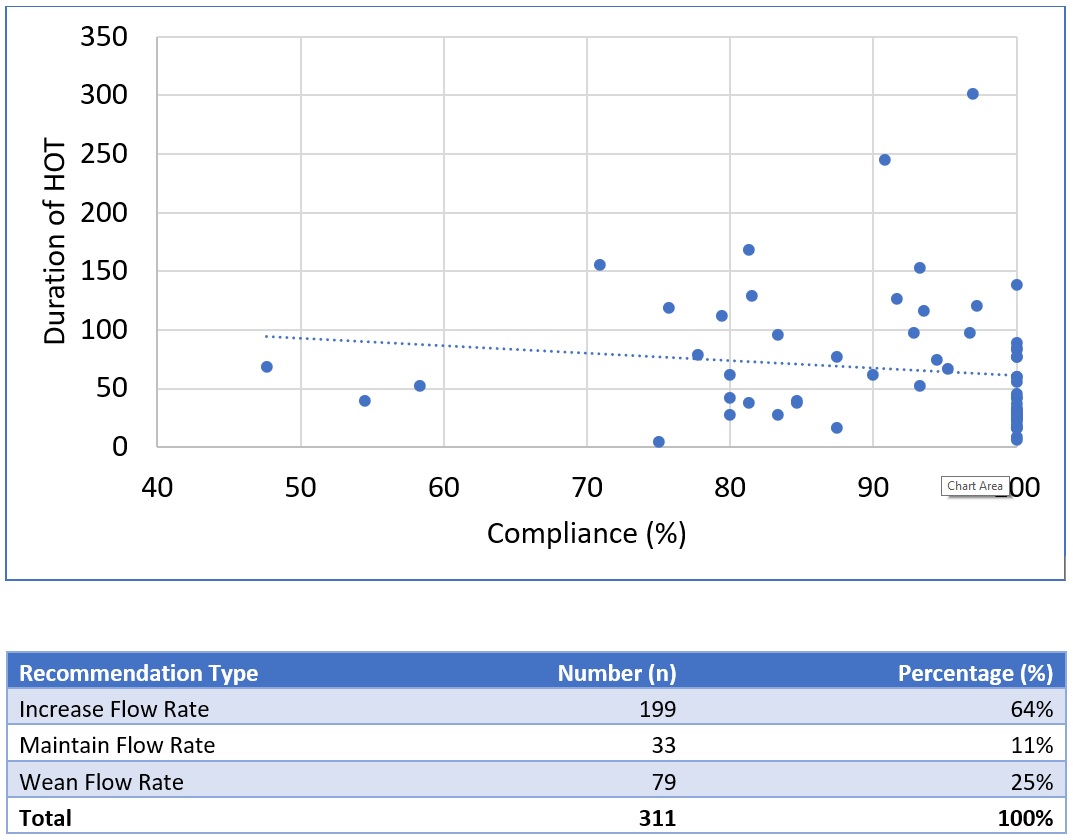
Objective: To describe the relationship between provider compliance with the RHO protocol, and the duration of HOT in premature infants.
Design/Methods: We conducted a prospective, multi-center implementation trial initiating the RHO Program as a management protocol for preterm infants on HOT at 14 U.S. academic medical centers. Infants were provided a WIFI-enabled pulse oximeter that wirelessly transmits recorded oximetry to a data coordinating center. Infants’ data was downloaded twice weekly, and providers were provided a recommendation to either decrease, maintain, or increase the current oxygen flow rate based on the original RHO Trial’s algorithm (Figure 1). Compliance with the algorithm’s recommendation was tracked. Compliance rates were calculated for each infant and duration of HOT was also collected.
Results: A total of 166 infants have been followed by the RHO Program across the 14 centers since implementation began in June 2021. 90% of infants have had an initial flow rate of 500 cc/min or less (Table 1). The average duration of HOT was 65.9 days (± 21.7 days) across sites with an average compliance rate of 91% (minimum compliance 47%; maximum 100%). Despite almost 2/3 of instances of non-compliance with the recommendation occurring when the algorithm suggests an increase in flow rate rather than a decrease, patients whose providers were compliant with algorithm recommendations actually had shorter durations of HOT. Durations of HOT in infants whose provider was greater than 90% compliant with protocol had an average duration of 65 days compared to 77 days in infants with lower compliance rates (p = 0.21) (Figure 2).
Conclusion(s): Higher rates of compliance with the RHO algorithm were associated with shorter durations of HOT in preterm infants followed by the RHO Program.
.jpg)
.jpg)
