Back
Background: With an increase in mental health visits to emergency departments, there has been an increase in aggressive patient behaviors that require interventions. The emergency department is typically a higher stress environment. During moments of high stress, patients and families can become upset for a variety of reasons. When this escalation occurs more resources are required, and a code gray is called. Trust-Based Relational Intervention (TBRI) techniques are skills used to de-escalate patients, particularly children and adolescents with a history of early stress, trauma, and abuse.
Objective: The objective of this study was to demonstrate a reduction in emergency department code grays as a result of de-escalation techniques.
Design/Methods: Pediatric Emergency Medicine Fellows and Attendings participated in an hour-long simulation based session on TBRI techniques. In each session, the participant was given the task of de-escalating aggression of a portrayed patient with various agitation triggers. Participants then underwent training on TBRI de-escalation techniques and the simulation was repeated. Patient data was collected on mental health patients, with exclusion of patients with diagnoses of autism spectrum disorders, psychosis, and acute intoxications, for both the 2 months preceding and 2 months post-simulation training. The differences in number of code grays called per 1,000 patient hours were compared.
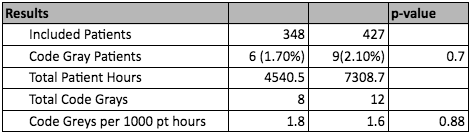
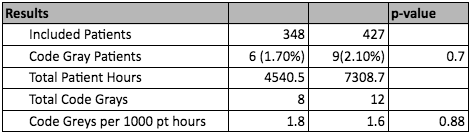
Results: The most common diagnoses for patients were depression and anxiety. The majority of patients were female, white, and non-Hispanic. Pre-simulation training included 348 patients with a total of 8 code grays called in 4,540.5 patient hours, accounting for 1.8 code grays per 1,000 patient hours. Post-simulation training included 427 patients with a total of 12 code grays called in 7,308.7 patient hours, accounting for 1.6 code grays called per 1000 patient hours.
Conclusion(s): The utilization of TBRI techniques demonstrated a slight reduction in code grays called per 1,000 patient hours from 1.8 to 1.6. Although this change was not statically significant (p-value 0.88), this reduction was noted during a time period of increased length of stays and ED admission holds due to demands on emergency department capacity. Of note is that there were multiple code grays called on excluded patients where TBRI techniques may not be effective. Next steps include expanding the pre- and post-training period analysis from 2 months to 6 months.
.png)
Emergency Medicine: All Areas
Emergency Medicine 6
361 - Trust-Based Relational Intervention (TBRI) Simulation Training for De-Escalation of Aggressive Patient in a Pediatric Emergency Department
Saturday, April 29, 2023
3:30 PM – 6:00 PM ET
Poster Number: 361
Publication Number: 361.21
Publication Number: 361.21
Daniel A. Castro, University of Texas at Austin Dell Medical School, Austin, TX, United States; Matthew Wilkinson, UT Austin Dell Medical School, Austin, TX, United States; Ada Earp, University of Texas at Austin Dell Medical School, Austin, TX, United States; Lina Palomares, Dell Children's Medical Center of Central Texas, Austin, TX, United States
Daniel A. Castro, MD (he/him/his)
Pediatric Emergency Medicine Fellow
University of Texas at Austin Dell Medical School
Austin, Texas, United States
Presenting Author(s)
Background: With an increase in mental health visits to emergency departments, there has been an increase in aggressive patient behaviors that require interventions. The emergency department is typically a higher stress environment. During moments of high stress, patients and families can become upset for a variety of reasons. When this escalation occurs more resources are required, and a code gray is called. Trust-Based Relational Intervention (TBRI) techniques are skills used to de-escalate patients, particularly children and adolescents with a history of early stress, trauma, and abuse.
Objective: The objective of this study was to demonstrate a reduction in emergency department code grays as a result of de-escalation techniques.
Design/Methods: Pediatric Emergency Medicine Fellows and Attendings participated in an hour-long simulation based session on TBRI techniques. In each session, the participant was given the task of de-escalating aggression of a portrayed patient with various agitation triggers. Participants then underwent training on TBRI de-escalation techniques and the simulation was repeated. Patient data was collected on mental health patients, with exclusion of patients with diagnoses of autism spectrum disorders, psychosis, and acute intoxications, for both the 2 months preceding and 2 months post-simulation training. The differences in number of code grays called per 1,000 patient hours were compared.
Results: The most common diagnoses for patients were depression and anxiety. The majority of patients were female, white, and non-Hispanic. Pre-simulation training included 348 patients with a total of 8 code grays called in 4,540.5 patient hours, accounting for 1.8 code grays per 1,000 patient hours. Post-simulation training included 427 patients with a total of 12 code grays called in 7,308.7 patient hours, accounting for 1.6 code grays called per 1000 patient hours.
Conclusion(s): The utilization of TBRI techniques demonstrated a slight reduction in code grays called per 1,000 patient hours from 1.8 to 1.6. Although this change was not statically significant (p-value 0.88), this reduction was noted during a time period of increased length of stays and ED admission holds due to demands on emergency department capacity. Of note is that there were multiple code grays called on excluded patients where TBRI techniques may not be effective. Next steps include expanding the pre- and post-training period analysis from 2 months to 6 months.
.png)
