Neonatal Infectious Diseases/Immunology
Neonatal Infectious Diseases/Immunology 2
669 - Neonatal anaerobe-targeted antibiotic therapy: Indications and utilization
Publication Number: 669.241
.jpg)
Matthew B. Green, MPH (he/him/his)
Medical Student
Rowan-Virtua School of Osteopathic Medicine
Voorhees, New Jersey, United States
Presenting Author(s)
Background:
Administration of anaerobe-targeted antibiotics (ATA) may be particularly impactful to the developing neonatal gut microbiome. Large-scale data on ATA therapy indications and utilization can inform ongoing neonatal antibiotic stewardship efforts. Repeated cross-sectional study including neonates admitted to a NICU from 2009-2021 in the Premier Database. ATA included piperacillin/tazobactam, metronidazole, clindamycin, cefoxitin, carbapenems, moxifloxacin, tigecycline, ampicillin/sulbactam, and ticarcillin/clavulanate. A course was defined as >4 consecutive days of parenteral administration. Clinical characteristics and ICD codes for diagnoses for which ATA therapy may be indicated (NEC/SIP, other GI anomaly/disorder, sepsis, and pneumonia/aspiration) were compared between neonates who received at least one ATA course and those who received only non-ATA courses, or no antibiotic course during hospitalization. We also compared outcomes between neonates who received 1 of 3 common ATAs (piperacillin-tazobactam, metronidazole, clindamycin). Annual antibiotic days of therapy (DOT; aggregate antibiotic days per 1000 patient days) for ATA, non-ATA and total therapy were assessed over time.
Objective: To assess indications for and utilization of anaerobe-targeted antibiotics among neonates admitted to the NICU.
Design/Methods:
Results:
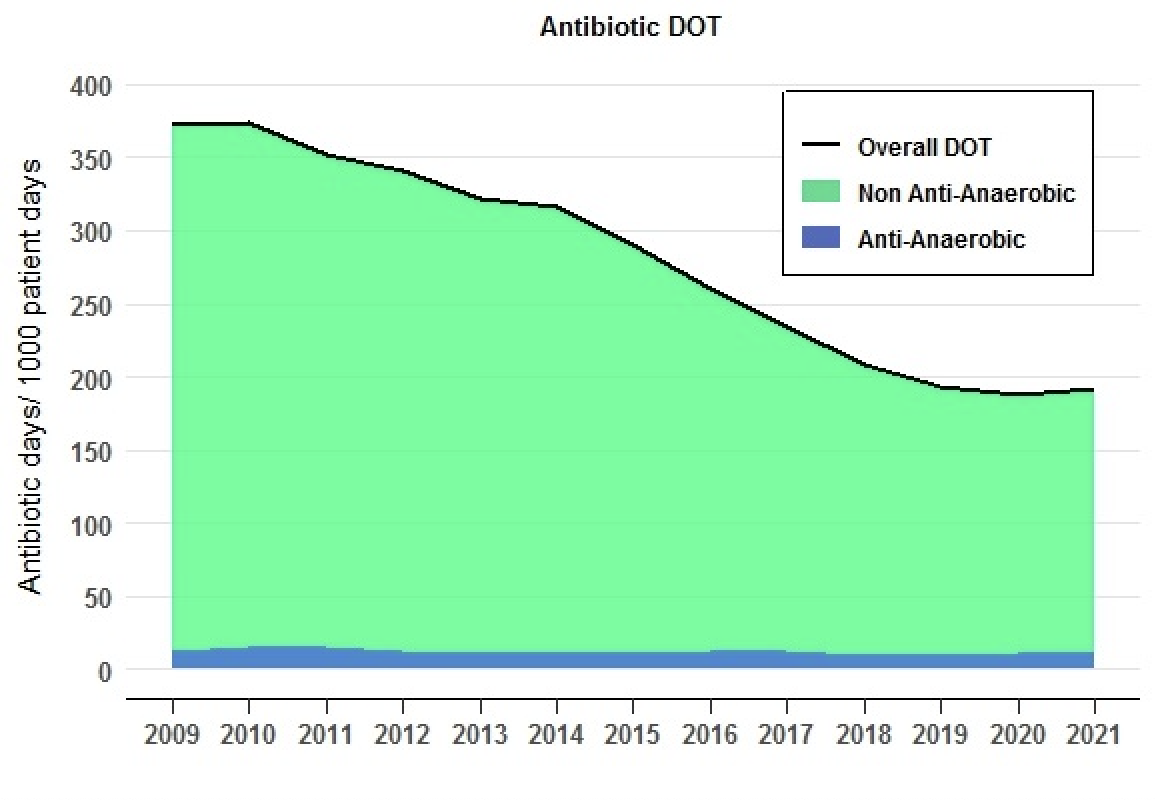
Of 1,395,791 neonates, 13,548 (1.0%) received an ATA course. Piperacillin-tazobactam was most commonly administered (5,037; 0.3%). Neonates administered an ATA course were more often very low birth weight (VLBW), had longer lengths of stay, and higher mortality compared to infants administered non-ATA course or no antibiotics (Table 1). Among neonates who received ATA, median first day of treatment after birth was 14 (IQR 6,28), and 10,268 (75.8%) had a possible indication based on ICD codes (Table 1). Neonates administered piperacillin-tazobactam were more often VLBW, differed in attributable ICD codes including less intestinal stricture, and had greater mortality than those treated with metronidazole or clindamycin (Table 2). Overall antibiotic DOT decreased over time, attributable to a decrease in non-ATA use, but ATA use remained unchanged. (Figure). This study of over 1.3 million neonates hospitalized from 2009-2021 suggests that many received ATA, though 1 in 4 cases did not have an attributable ICD code. Although overall antibiotic and non-ATA use decreased over time, ATA use remained unchanged. Given their impact on the developing gut microbiome, further research should assess the optimal indications and utility of ATA.
Conclusion(s): 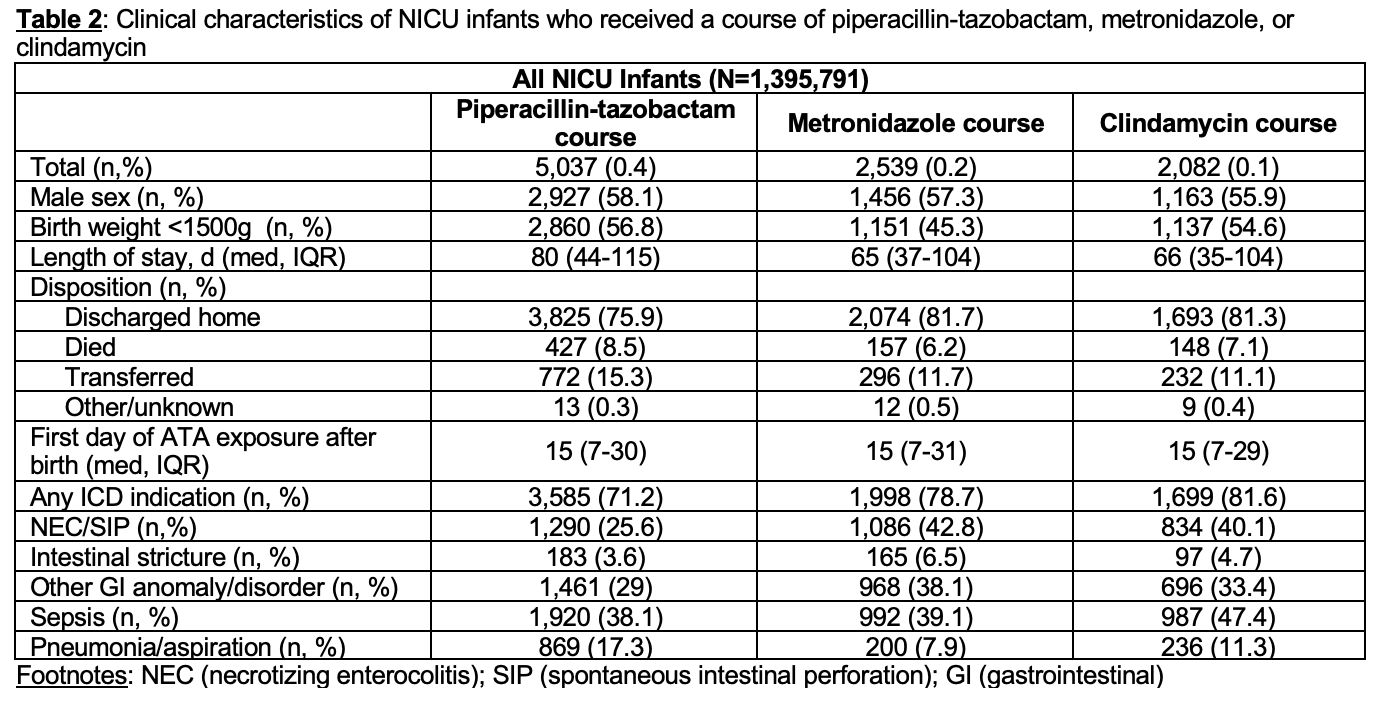
.png)