Adolescent Medicine: Substance Use
Adolescent Medicine 2
13 - Severe and life-threatening opioid, stimulant and sedative use in Canadian youth: a one-time survey of paediatricians and paediatric subspecialists
Publication Number: 13.2

Matt Carwana, MD MPH FRCPC (he/him/his)
Clinical Assistant Professor, Department of Pediatrics
University of British Columbia Faculty of Medicine
Vancouver, British Columbia, Canada
Presenting Author(s)
Background:
Toxic drug supply is a public health emergency. The syndemic impact of Covid-19 has exacerbated the adverse outcomes of overdose, driving up mortality rates. Despite the fact that opioid use disorder is predominantly viewed as an adult issue, an increasing number of youth in Canada experience severe-life threatening overdose; it is the leading cause of death in youth ages 10-18 in Western Canada. Epidemiologic data related to this population remains limited.
Objective:
1. Determine the minimum incidence of children and adolescents presenting with severe/life-threatening opioid, stimulant and sedative exposure among youth presenting to Canadian paediatricians and paediatric subspecialists
2. Describe the treatment and services available for youth presenting with substance use to paediatric care in Canada
Design/Methods:
A one-time cross-sectional survey of Canadian paediatricians and paediatric subspecialists using the Canadian Paediatric Surveillance System (CPSP) was conducted in the Spring of 2022. A population denominator of 2,900,866 was selected based on Statistics Canada census data for children and youth 12-18 in 2021. Data were analyzed using Stata v15.1.
Results:
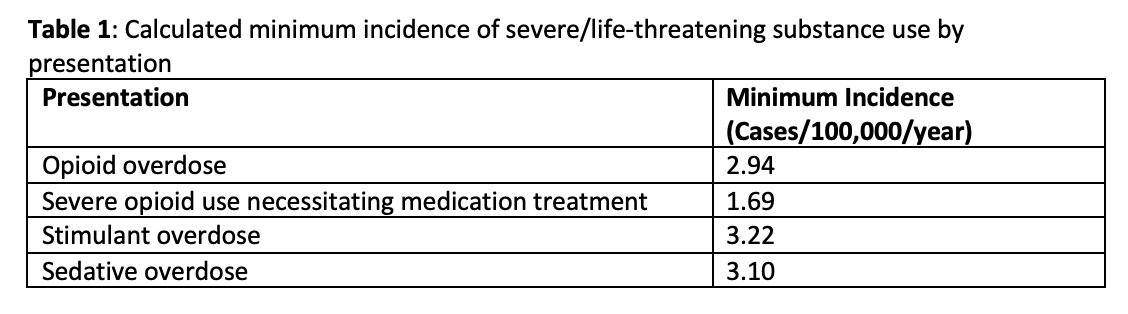
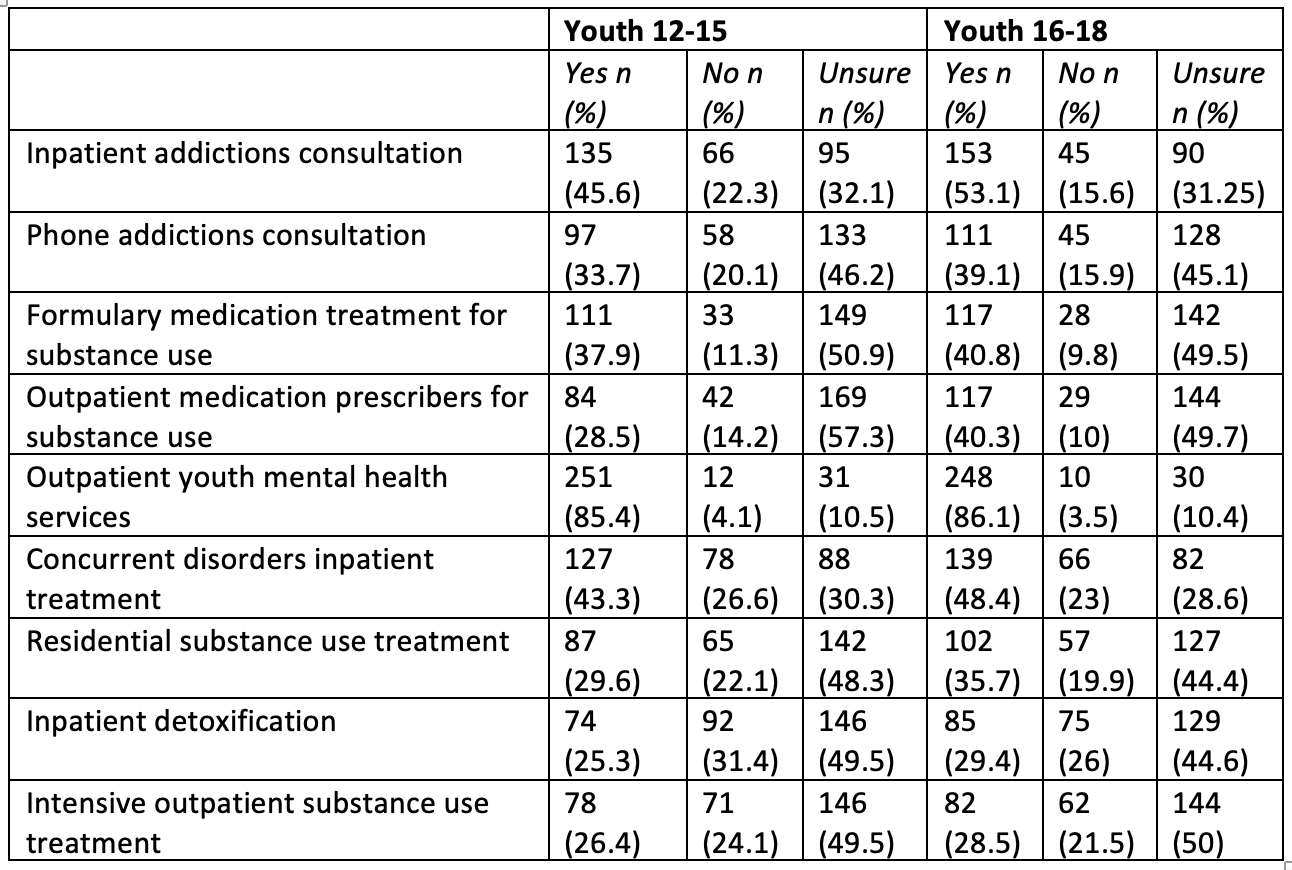
1027 respondents (response rate: 37%) completed the survey, of whom 934 (90.9%) reported providing care to children and youth 12 years and above. 115 (12.3%) respondents indicated managing a youth with severe or life-threatening substance use in the prior 24 months. Most providers operated in urban settings (n=95, 84.8%), but there were cases reported in suburban (n=9, 8.0%) and rural/remote (n=8, 7.1%) environments as well. Calculated minimum cumulative incidence per 100,000/year were: opioid overdose 2.94; opioid use requiring pharmacotherapy 1.69; stimulant toxicity 3.22; and sedative toxicity 3.1 (Table 1). Respondents also reported service availability for youth substance use. Respondent awareness of availability of overdose-related services was high for outpatient mental health services (85.4% for 12-15-year-olds, 86.1% for 16-18-year-olds), but poor to moderate (25.3%-53.1%) for all other surveyed services including inpatient stabilization and intensive outpatient management.
Conclusion(s):
Paediatricians and subspecialists interface significantly with youth with severe substance use and overdose. There minimum calculated incidence rates provided are significant and concerning at the population level, despite excluding youth that do not seek physician care after overdose. Paediatric providers have limited awareness of service availability for youth that use substances. Further studies and knowledge translation are required.