Nephrology: Clinical
Nephrology 1: AKI
253 - Does a Tincture of Time Change CRRT Practice and Improve outcomes: A comparison of the ppCRRT and WE-ROCK collaboratives
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 253
Publication Number: 253.25
Publication Number: 253.25
Shina Menon, University of Washington School of Medicine, Seattle, WA, United States; David Selewski, Medical University of South Carolina, Mount Pleasant, SC, United States; Scott Sutherland, Stanford University School of Medicine, Palo Alto, CA, United States; Theresa A. Mottes, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Stuart L. Goldstein, Cincinnati Children's Hospital, Cincinnati, OH, United States; Katja M. Gist, Children's Hospital Medical Center (Cincinnati), Cincinnati, OH, United States

Shina Menon, MD (she/her/hers)
Associate Professor
University of Washington School of Medicine
Seattle, Washington, United States
Presenting Author(s)
Background: There are limited data regarding the epidemiology of pediatric patients receiving continuous renal replacement therapy (CRRT). The Prospective Pediatric continuous renal replacement therapy (ppCRRT) Registry (13 centers in the United States, n=344), which described practice patterns and outcomes almost two decades ago, was previously the largest cohort of children receiving CRRT. The Worldwide Exploration of Renal Replacement Outcomes Collaborative in Kidney Disease (WE-ROCK, 32 centers, 7 countries, n=992) registry was designed to update the current international practice patterns for pediatric CRRT
Objective: This study aims to evaluate changes in population characteristics and outcomes across these 2 cohorts
Design/Methods: We performed a retrospective cohort analysis comparing patient characteristics, CRRT prescription, and outcomes between the ppCRRT and WE-ROCK registries. The WE-ROCK study included children aged 0-25 years treated with CRRT for AKI or FO, and patients with previous dialysis dependence, ECMO utilization, or who received CKRT for non-AKI/fluid overload were excluded. Thus, for this analysis, patients with inborn errors of metabolism were excluded from the ppCRRT registry
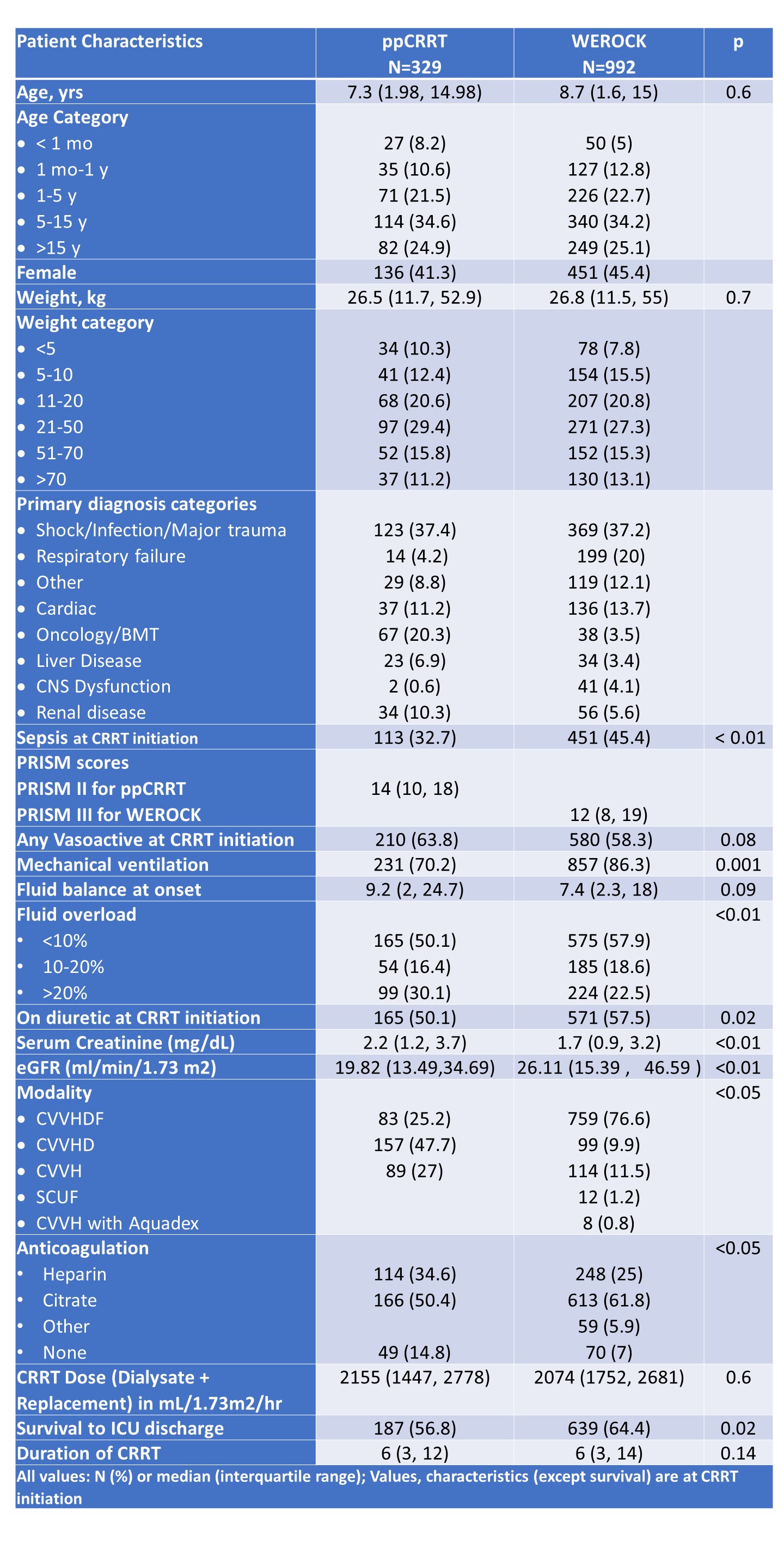
Results: Data from 992 children from WE-ROCK were compared with 329 from ppCRRT. There were no differences in the median age, sex or weight of patients between the cohorts (Table 1). The most common reason for admission was shock, infection, or major trauma (37.2% vs 37.4%). Sepsis was more common in the WE-ROCK cohort (45.4%) thatn the ppCRRT cohort (32.7%, p< 0.01). Although the median fluid balance at CRRT initiation was not significantly different between the cohorts ( 7.4 vs. 9.2 WEROCK vs ppCRRT, p 0.09), fewer patients started CRRT with > 20% fluid overload in the WE-ROCK cohort (22.5% vs 30.1%, p < 0.01).
The prescribed CRRT dose was similar across the cohorts (2074 mL/1.73 m2/hour compared to 2155). However the use of convective modalities was higher in the WE-ROCK cohort (88.1% vs. 52%, p< 0.05), as was the use of regional citrate anticoagulation (61.8% vs 50%, p < 0.05).
Survival to ICU discharge was seen in 64.4% of WEROCK cohort compared to 56.8% of ppCRRT (p 0.02)
Conclusion(s): Comparison of WE-ROCK with the older ppCRRT cohort shows changes in CRRT practice patterns and higher survival rates. This may be related to better recognition of fluid overload as the proportion of patients who had > 20% FO at CRRT initiation has decreased. However given the retrospective nature of WEROCK, it is not possible to draw definitive conclusions and other causes need to be studied