Neonatal General
Neonatal General 5: COVID, Infections Diseases
699 - A Modified Observational Approach to Infants Born to Mothers with Chorioamnionitis Reduces Antibiotic Exposure and NICU Admission
Publication Number: 699.233

Cynthia S. Liang, MD, MBA (she/her/hers)
Resident Physician
UPMC Children's Hospital of Pittsburgh
PITTSBURGH, Pennsylvania, United States
Presenting Author(s)
Background:
Term infants born to mothers with chorioamnionitis are at increased risk of early onset sepsis (EOS). In February 2021, our institution changed its protocol for managing well-appearing term infants born to mothers with chorioamnionitis from a categorical approach for determining antibiotic use to a modified observation-based approach following an initial lab evaluation. We aimed to safely decrease antibiotic use while still ensuring rapid identification of newborns with EOS.
Objective:
Measure the impact of an observation-based approach for evaluating term infants of mothers with chorioamnionitis on antibiotic utilization, NICU utilization, and hospital costs.
Design/Methods:
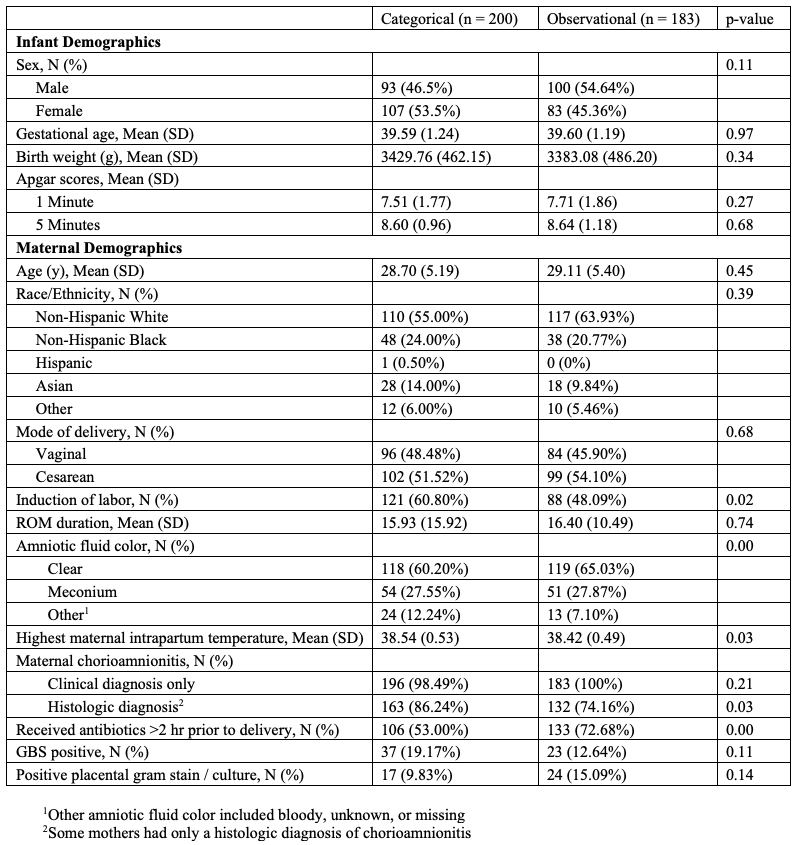
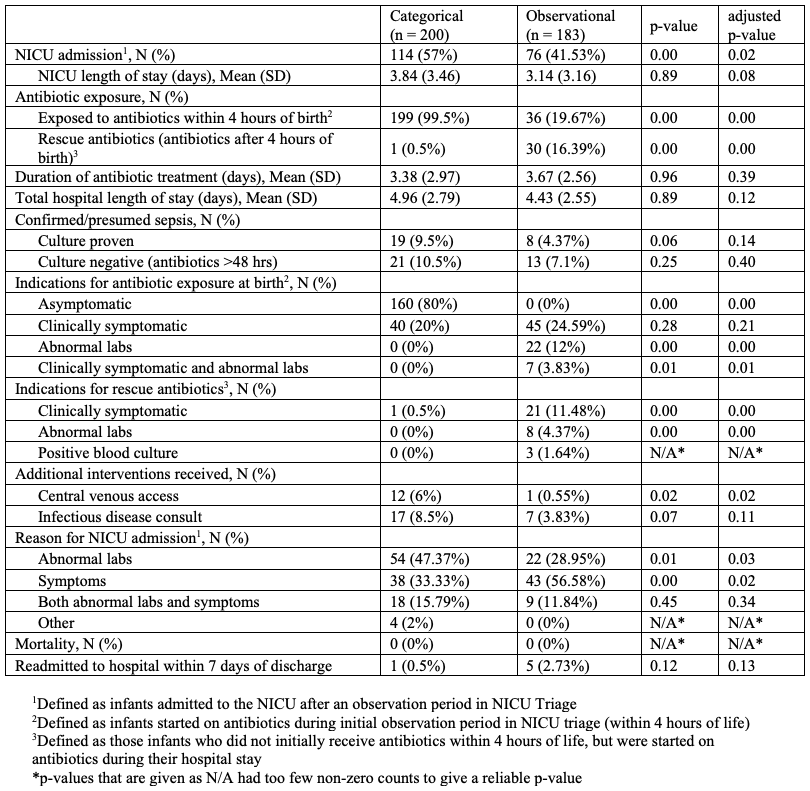
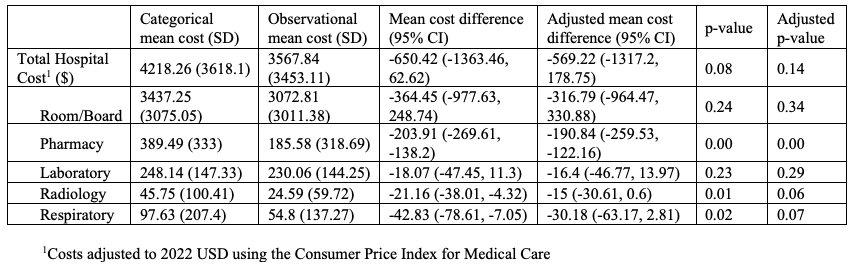
We conducted a retrospective pre-post cohort study of term infants born to mothers with chorioamnionitis at a single center during two periods (categorical period: 2/1/2019 – 1/31/2020; observational period: 2/1/2021 – 1/31/2022). Infants with congenital anomalies or alternate indications for NICU admission were excluded. Clinical data were collected from retrospective chart review and prospective documentation after the practice change. Hospital costs were estimated using cost-to-charge ratios for hospital billing during the newborn birth hospitalization. Primary outcomes included antibiotic exposure, NICU admission, and hospital costs. Analyses with binary and continuous outcomes were performed using logistic regression and ordinary least squares, respectively, where "adjusted" analyses adjusted for demographic variables. P-values were computed using likelihood ratio tests. Confidence intervals were standard Wald-type intervals. Analyses were done using R v4.1.2.
Results:
383 term infants were included (200 in the categorical cohort; 183 in the observational cohort). Demographic and clinical outcomes are summarized in Tables 1 and 2, respectively. There was a significant decrease in NICU admission and antibiotic exposure (p < 0.05) in the observational cohort. However, for infants that received antibiotics, there was no difference in duration of antibiotic therapy between the two groups. There was also no difference in confirmed/presumed sepsis, positive blood cultures, total hospital length of stay, or NICU length of stay between the two groups. Cost data is summarized in Table 3. The observational cohort saw a significant decrease in some hospital costs including pharmacy, radiology, and respiratory costs (p < 0.05) but not in total hospital costs.
Conclusion(s):
An observation-based approach to evaluating term infants of mothers with chorioamnionitis is a safe way to reduce unnecessary antibiotic therapy and NICU admission.