Neonatal Hematology & Bilirubin Metabolism
Neonatal Hematology & Bilirubin Metabolism 2: Hematology
134 - Associations between blood donor sex and age, and outcomes of transfused newborn infants
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 134
Publication Number: 134.239
Publication Number: 134.239
Timothy M. Bahr, Intermountain Healthcare/University of Utah, Salt Lake City, UT, United States; Thomas R. Christensen, University of Utah, Salt Lake City, UT, United States; Sarah 78259, University of Utah School of Medicine, Salt Lake City, UT, United States; Erick Henry, Intermountain Healthcare, Murray, UT, United States; Terry Rees, Intermountain Medical Center, Murray, UT, United States; Mark Astin, Intermountain Healthcare Transfusion Services, Kaysville, UT, United States; walter Kelley, University Arizona College of Medicine, Alpine, UT, United States; Sarah J.. Ilstrup, Intermountain Healthcare Central Laboratory, Park City, UT, United States; Robin K. Ohls, University of Utah School of Medicine, Salt Lake City, UT, United States; Robert D. christensen, University of Utah School of Medicine, Salt Lake City, UT, United States

Timothy M. Bahr, MD
Assistant Professor
Intermountain Healthcare/University of Utah
Salt Lake City, Utah, United States
Presenting Author(s)
Background: It is controversial whether the sex of red blood cell (RBC) donors or the age of the donor affects mortality or morbidities of transfused newborn infants.
Objective: We evaluated whether the sex or age of red blood cell (RBC) donors affected mortality or morbidities of transfused newborn infants using a multi-year, multi-hospital database linking specific outcomes of neonatal transfusion recipients with RBC donor sex and age.
Design/Methods: We performed retrospective analyses of all neonates receiving ≥ one RBC transfusion during a 12-year period in all Intermountain Healthcare hospitals, matching mortality and specific morbidities of each transfusion recipient with the sex and age of each donor.
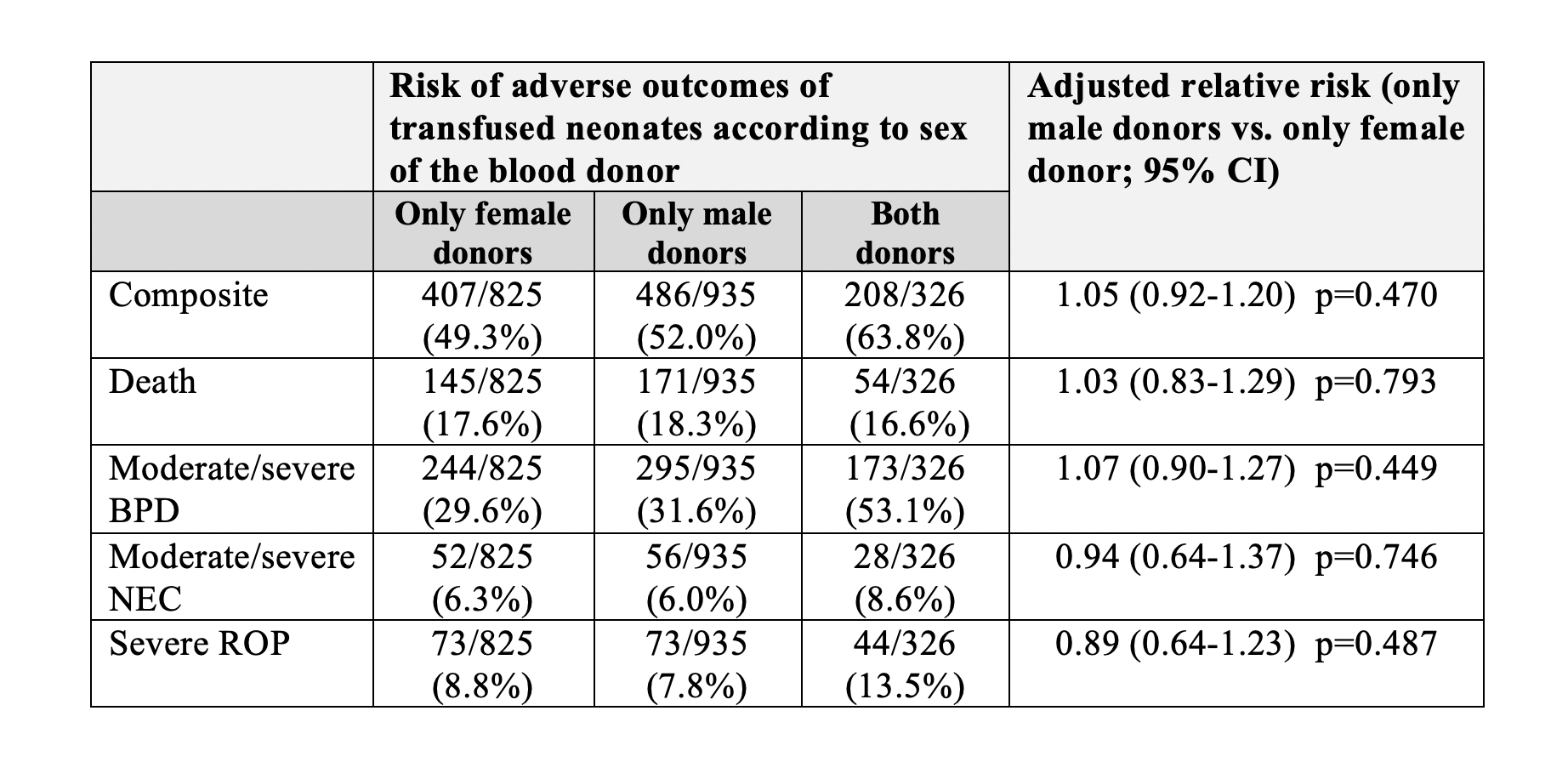
Results: There were 6,396 RBC transfusions administered to 2,086 infants in 15 hospitals. A total of 825 infants were transfused exclusively with RBC from female donors, 935 infants were transfused exclusively with RBC from male donors, and 326 infants were transfused with RBC from both female and male donors. No differences in baseline characteristics were identified among the three groups. Infants who received blood from both male and female donors had more RBC transfusions: 5.3±2.9 transfusions if the infant received both male and female donor blood vs. 2.6±2.2 if the infant received blood from only one sex, mean±SD, p< 0.001. We identified no significant differences in mortality or selected morbidities (bronchopulmonary dysplasia, necrotizing enterocolitis, or retinopathy of prematurity) associated with the sex or the age of donors (Table 1). Similarly, an analysis of matched vs. mismatched donor/recipient sex revealed no associations with death or neonatal morbidities.
Conclusion(s): These data support the practice of transfusing newborn infants with RBC obtained from donors of either sex, and from donors of any age.