Neonatal Fetal Nutrition & Metabolism
Neonatal GI Physiology & NEC 4: Gut Health, Enteral Nutrition and Oral Feeding
87 - Outcomes of an Exclusive Human Milk Diet in Infants with Congenital Gastrointestinal Disorders
Publication Number: 87.236

Heidi E. Karpen, MD (she/her/hers)
Associate Professor of Pediatrics
Emory University/Children's Healthcare of Atlanta
Atlanta, Georgia, United States
Presenting Author(s)
Background:
Human milk (HM) is considered the ideal source of nutrition for all infants but often falls short in meeting the protein and energy needs of infants with congenital gastrointestinal disorders (CGD) requiring surgical intervention. These infants have high rates of postnatal growth failure which can have long-lasting effects on neurodevelopment. Currently, the only option for these infants is fortification with formula products, which carries its own risk for deleterious outcomes such as necrotizing enterocolitis (NEC).
Objective:
Primary objective was to compare time to full enteral feedings and days on parenteral nutrition (PN) between those fed an EHMD compared with those fed partial and non-human milk diets. Secondary objectives included peak conjugated bilirubin levels, incidence of sepsis, feeding intolerance/interruptions, necrotizing enterocolitis (NEC), death, and length of stay.
Design/Methods: This was a matched, case-controlled, comparative effectiveness trial of infants with CGD (gastroschisis, omphalocele, and intestinal atresia). The treatment cohort (n=151) was fed an exclusive human milk diet (EHMD) of mother’s own milk (MOM), pasteurized donor human milk (PDHM) fortified with one of two human milk-based fortifiers (HMBF): H2MF® for those < 37 weeks’ gestational age (GA) or PBCLN-002, a novel HMBF specifically formulated for the term infant. Comparison group (n+151) was a 1:1 ratio, propensity-matched, recent retrospective control cohort receiving formula or bovine milk–based fortifier as part of their diet.
Results:
As compared with those in the control group, infants fed an EHMD following surgical repair experienced shorter time to reach full enteral feeds (Kaplan-Meier estimate of median: 32 vs 44 days, respectively; p< 0.0001; all CGD, N=302). EHMD fed infants had: lower peak conjugated bilirubin including lower maximum direct bilirubin (median±IQR: 0.7±1.3 vs 1.0±2.0 mg/dL respectively; p< 0.003); lower incidence of NEC
[n (%): 3.0 (2.0) vs 11 (7.3), respectively, p=0.03]; greater weight gain velocity (mean ± SD: 20.9 ± 9.6 vs 17.4 ± 12.1 g/d, respectively, p=0.02) and less negative change in weight z score from birth to discharge (mean±SD: -0.53±0.74 vs -0.84±0.70, respectively, p=0.0002) as compared with the control group.
Conclusion(s):
EHMD intervention was safe and well-tolerated in all CGD infants. As compared with controls, CGD infants receiving the EHMD experienced shorter time to full enteral feeds, had a substantially decreased incidence of NEC, lower peak conjugated bilirubin, and improved weight gain compared to controls fed partial or exclusive bovine-based diets. 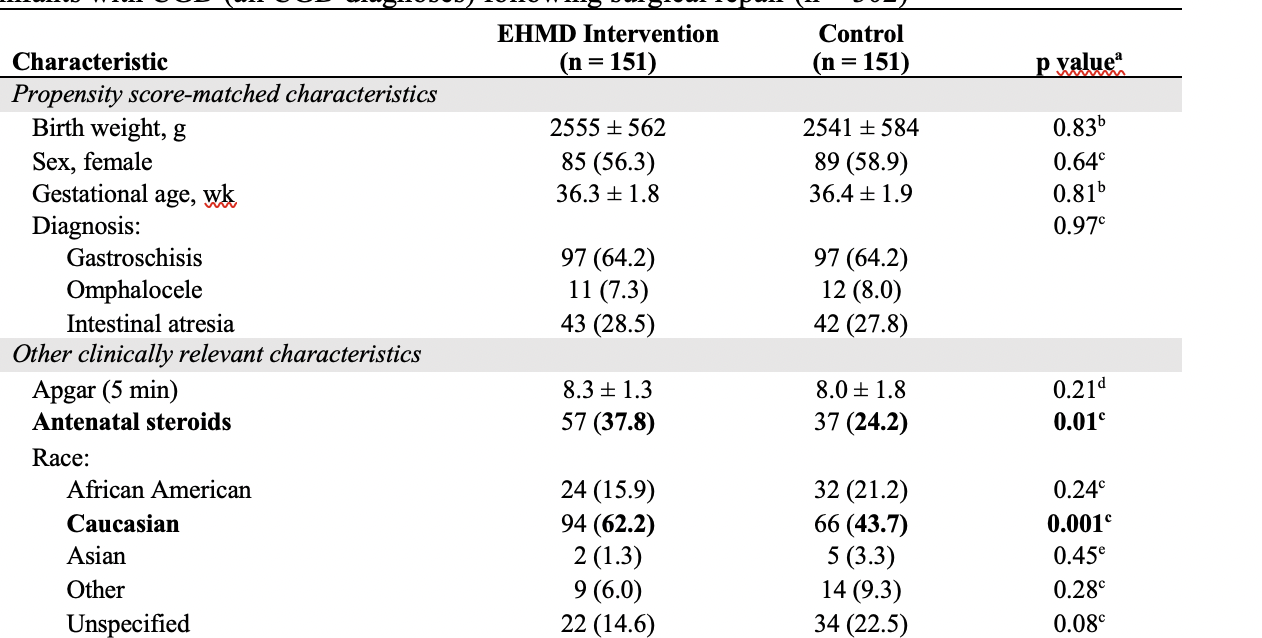
.png)
