General Pediatrics: Primary Care/Prevention
General Pediatrics 4
474 - Instrument-Based Vision Screening at Well-Child Checks: Implementation Within a Children’s Hospital System
Publication Number: 474.217
- EH
E Eugenie Hartmann, PhD (she/her/hers)
Senior Research Scientist
Akron Children's Hospital
Akron, Ohio, United States
Presenting Author(s)
Background:
Amblyopia is the result of abnormal neural development in the visual cortex of the brain that leads to reduced visual acuity in one eye, relative to the other eye (monocular amblyopia); or in both eyes, relative to normal (bilateral amblyopia). Vision screening at Well-Child-Checks is especially important during the preschool years to identify children with amblyopia or risk factors for amblyopia, because treatment is most effective during this time period. Since the mid-1990s camera-like instruments (photo screeners) have been used to quantify the blurriness or clarity of an image by estimating the refractive correction required to yield optimal focus of light directly onto the retina. This information can be translated into risk factors for impaired vision and hence indicate when a referral to an eye care provider is warranted.
Objective:
The purpose of this report is to summarize the system-wide use of a photo-screening instrument for vision assessments at the 3-, 4- and 5-year Well Child Checks (WCC) in pediatric offices.
Design/Methods:
From April through December 2021, 34 Akron Children’s Hospital Pediatric (ACHP) clinics were equipped with the Welch Allyn SPOT Vision Screener. In person instructions were given to both staff and providers at each office by the first author (EEH). Presentations included background information about the purpose of vision screening and the detection of amblyogenic risk factors by the device, as well as hands-on practice. Work flow in the EPIC Electronic Health Records was modified so that SPOT vision screening was automatically ordered for all 3-, 4- and 5-year WCCs with both results and referrals easily entered.
Results:
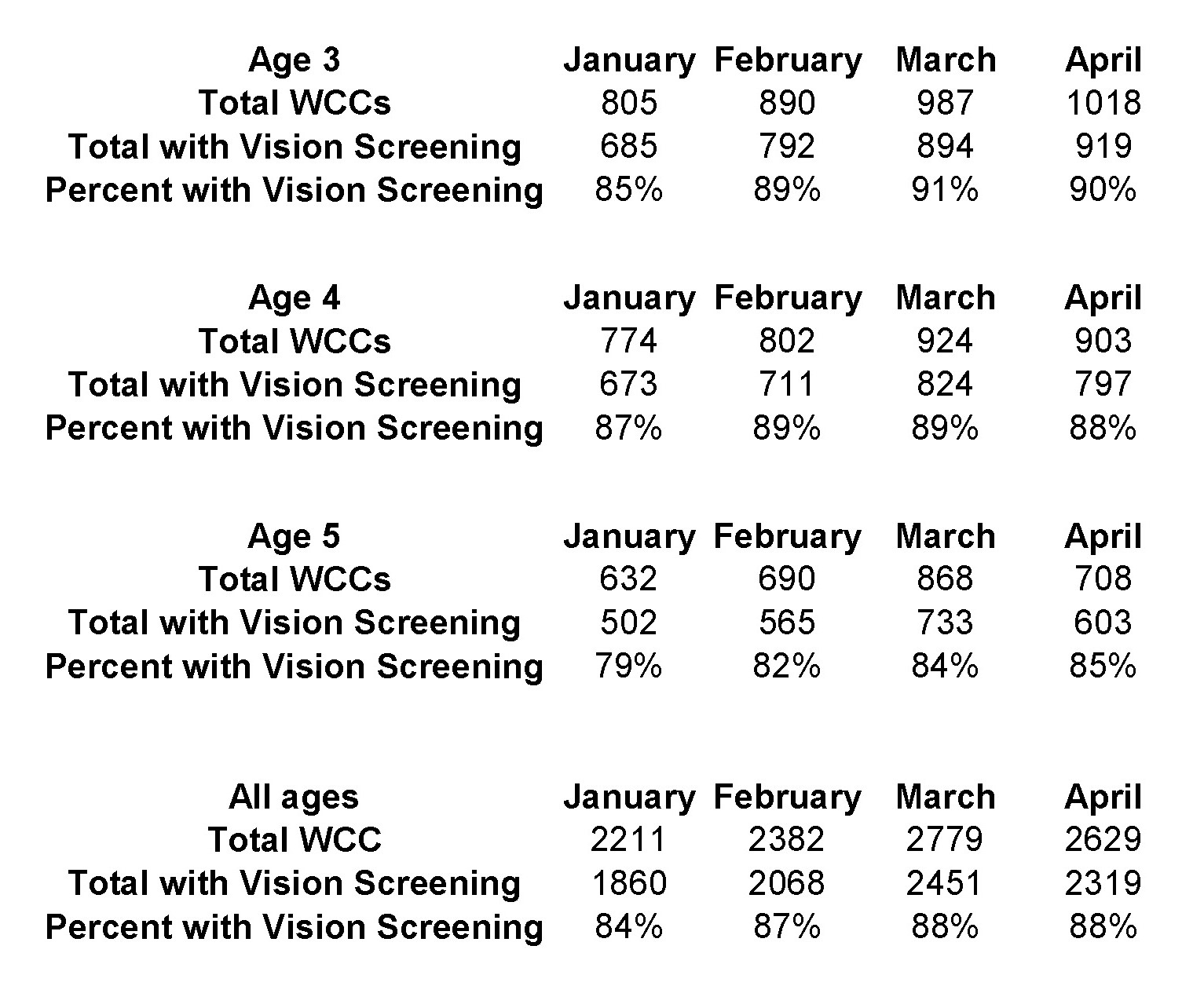
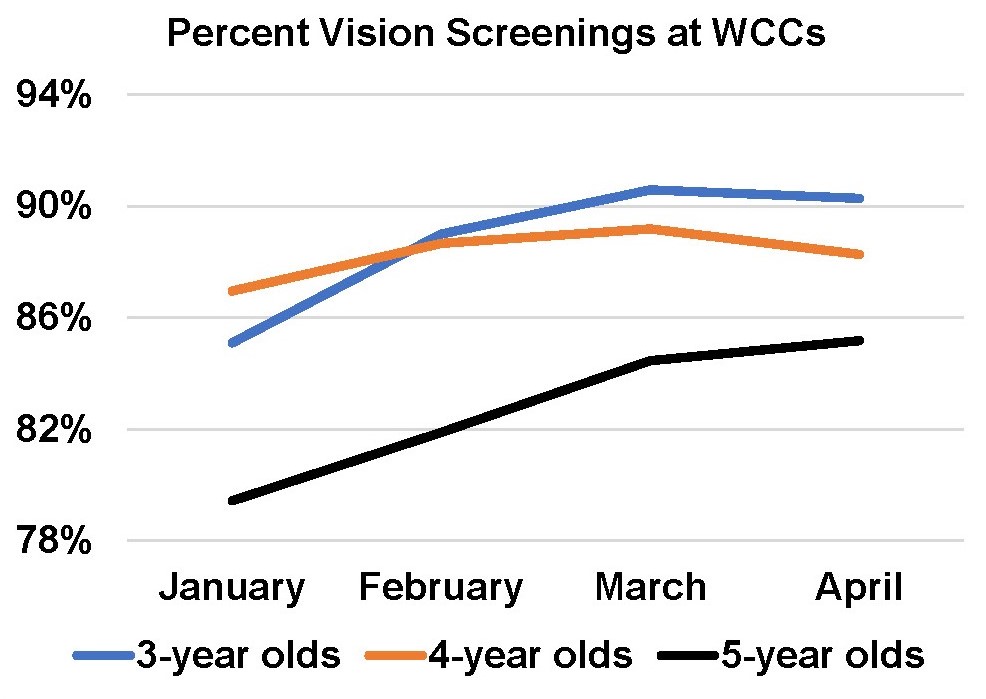
The number of WCCs by age group during the first four months of 2022 (January-April) was 3,700 for 3-year olds; 3,403 for 4-year olds and 2,898 for 5-year olds. Vision screenings were completed on 89% of 3-year olds; 88% of 4-year olds and 83% of 5-year olds. The number of referrals for a comprehensive eye examination was 504 (15%) for 3-year olds; 420 (14%) for 4-year olds and 299 (12%) for 5-year olds.
Conclusion(s):
Although staff compliance with the new protocol varied across sites, ranging from 53 to 100%, the average compliance improved from January to April (84 to 88%). The similarity between screening rates at ages 3 and 4 is encouraging, given the challenges of successful vision screening with these young children. This project has demonstrated the feasibility of employing new technology for vision screening of preschool-aged children within a large Children’s Hospital system.