Neonatal Nephrology/AKI
Neonatal Nephrology/AKI 1
219 - Timing and Risk factors associated with Acute Kidney Injury (AKI) in infants with Necrotizing Enterocolitis (NEC)
Publication Number: 219.242
.jpg)
Geethanjali Lingasubramanian, MD
PGY6 Neonatology Fellow
Rutgers, Robert Wood Johnson Medical School
New brunswick, New Jersey, United States
Presenting Author(s)
Background: NEC remains a leading cause of morbidity and mortality among premature neonates and the pathogenesis of this disease is likely multi-factorial. Recent studies have shown an increased mortality rate and length of stay (LOS) in neonates with NEC, associated with AKI. In most of these studies, onset of AKI was noted to be soon after NEC diagnosis. Only a few studies have evaluated the association between NEC and AKI, with varying study results, thus necessitating further research.
Objective:
To evaluate the prevalence, time of onset and the risk factors associated with AKI in infants with NEC. In addition, to assess the impact on the length of stay (LOS) and mortality rate in patients with NEC with/without AKI.
Design/Methods:
This study was conducted at The Children’s Regional Hospital at Cooper, a Level IIIB urban in-born and referral neonatal intensive care unit (NICU). A retrospective chart review of infants < 32 weeks of gestation and birth weight < 1500 grams born between January 2011 to December 2021with definite NEC (diagnosed using modified Bell’s staging ≥ Stage 2) was done. In these infants, we identified those with AKI, using the modified neonatal Kidney Disease: Improving Global Outcomes criteria (KDIGO) criteria. The timing of AKI onset in relation to NEC onset was obtained by trending serum creatinine and urine output values. Demographics and clinical variables were compared between the two groups of infants with NEC, with and without AKI. Mortality rate and LOS were the primary outcomes of this study. Statistical tests used for analysis were Independent t tests, Mann Whitney U, Chi square, and Fisher Exact tests.
Results:
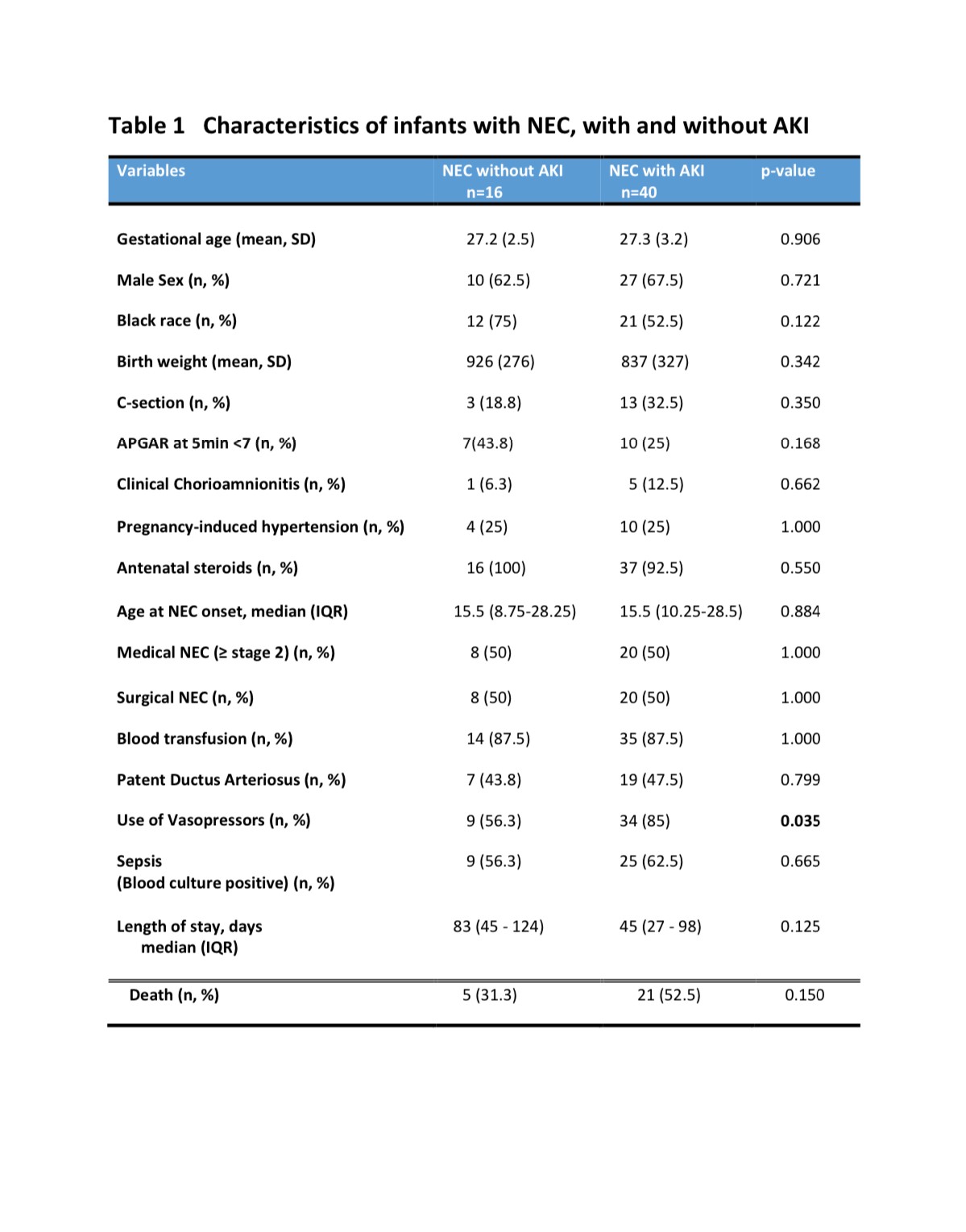
Among 56 eligible infants, 40 (71%) had AKI of any stage. Six (15%) had stage 1, 17 (42.5%) had stage 2 and 17(42.5%) had stage 3 AKI. AKI onset coincided or occurred prior to the onset of NEC (median AKI onset was one day prior to onset of NEC, interquartile range -3 to 0 days). Table 1 shows the comparison of the NEC infants with or without AKI. Vasopressors were significantly more likely to be used in infants having NEC with AKI (p=0.035; Table 1). There was no statistically significant difference in mortality rate or LOS between the groups.
Conclusion(s):
Onset of AKI mostly precedes NEC onset, with moderate to severe AKI more prevalent than milder form in infants with NEC. These infants are significantly more likely to be hemodynamically unstable, requiring vasopressors. No significant increase in mortality rate or LOS was noted between the groups.