Neonatal General
Neonatal General 6: Neurology
709 - Characterizing cerebral blood flow and its alterations from packed red blood cell transfusion during the first week of life in premature infants
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 709
Publication Number: 709.234
Publication Number: 709.234
Manas Tetarbe, Keck School of Medicine of the University of Southern California, Glendale, CA, United States; Manoj Biniwale, Keck School of Medicine of the University of Southern California, Los Angeles, CA, United States; Deepti Nagesh, Children's Hospital of Los Angeles, Los Angeles, CA, United States; Rangasamy Ramanathan, Keck School of Medicine of USC, Los Angeles, CA, United States; Tai-Wei Wu, Division of Neonatology, Fetal and Neonatal Institute, Children’s Hospital Los Angeles, Department of Pediatrics, Keck School of Medicine of USC, Los Angeles, California, United States, Los Angeles, CA, United States

Manas Tetarbe, D.O.
Neonatal-Perinatal Medicine Fellow
Keck School of Medicine of the University of Southern California
Glendale, California, United States
Presenting Author(s)
Background: Intraventricular Hemorrhage (IVH) is the most common type of intracranial hemorrhage in premature infants. Packed red blood cell (PRBC) transfusion during the first week of life is an independent risk factor for the development of IVH.
Objective: To characterize cerebral blood flow (CBF) patterns in the first week of life in relation to hemoglobin concentration and PRBC transfusion in the first week of life in infants born at ≤32 weeks gestation.
Design/Methods: This was a prospective study involving infants born at ≤32 weeks gestation. Cerebral blood flow velocities (CBF) in the left middle cerebral artery (MCA), including peak-systolic velocity (PSV), end-diastolic velocity (EDV), and mean velocity (MV) were measured by transcranial Doppler ultrasound. Baseline CBFs were obtained on day of life (DOL) 1, 2 and 3, in addition to peri-transfusion measures at 4 time points (pre-transfusion, mid-transfusion, end-transfusion, and 24 hours post-transfusion). The decision to perform a PRBC transfusion was at the discretion of the clinical team. RM-ANOVA and mixed-effects analysis were used to detect changes in variables over time. Post-hoc Tukey testing identified significant changes between time points.
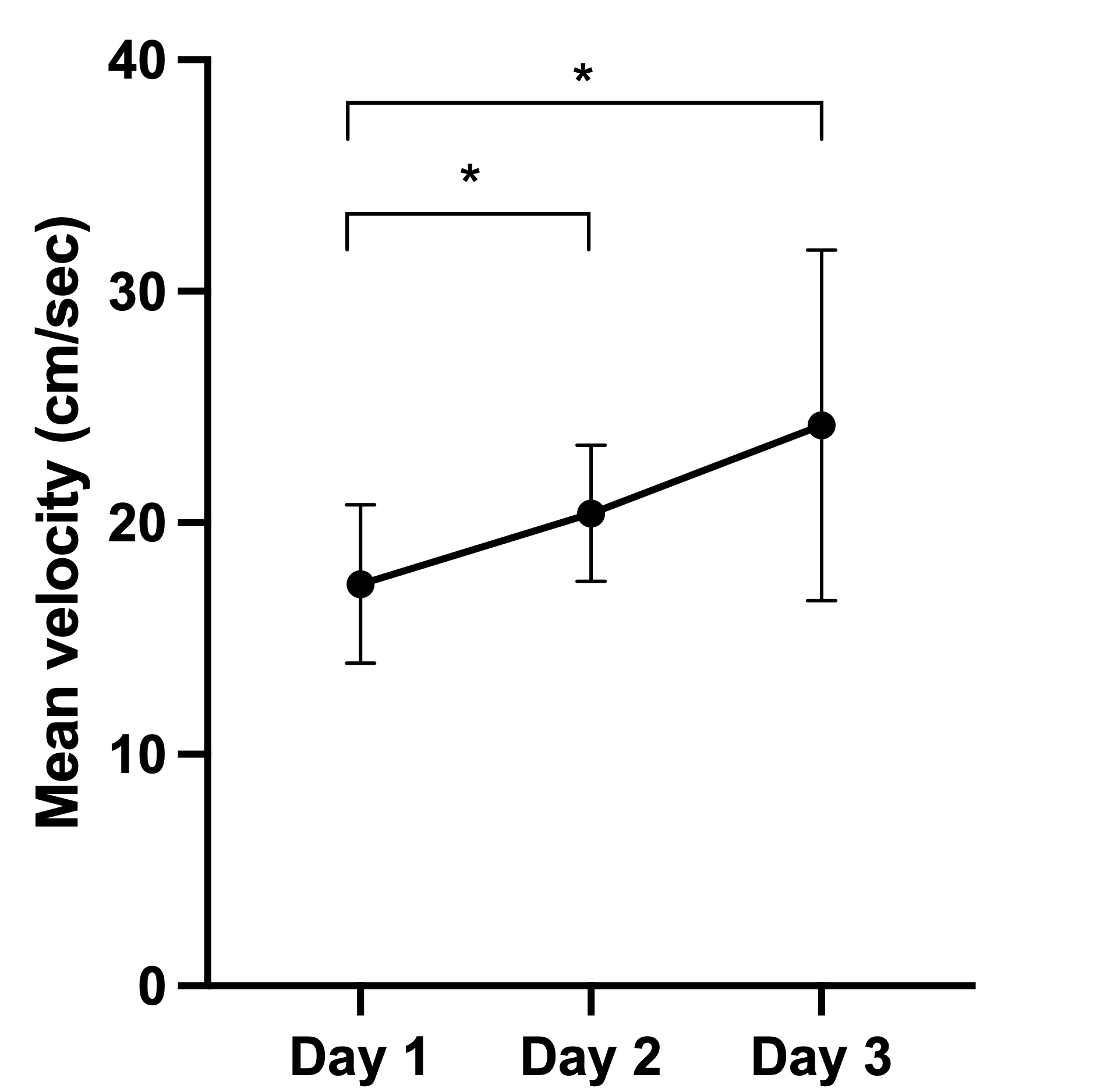
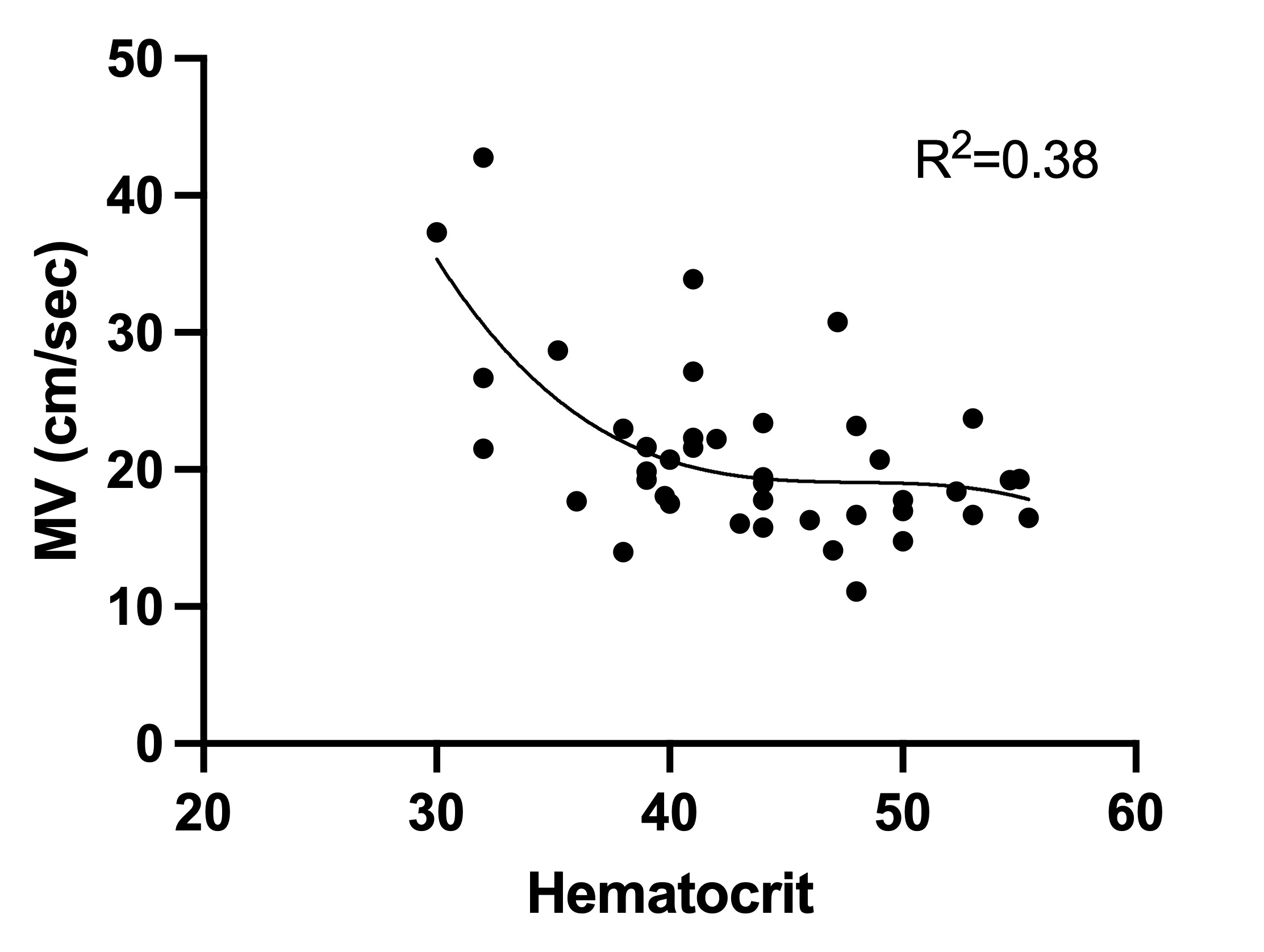
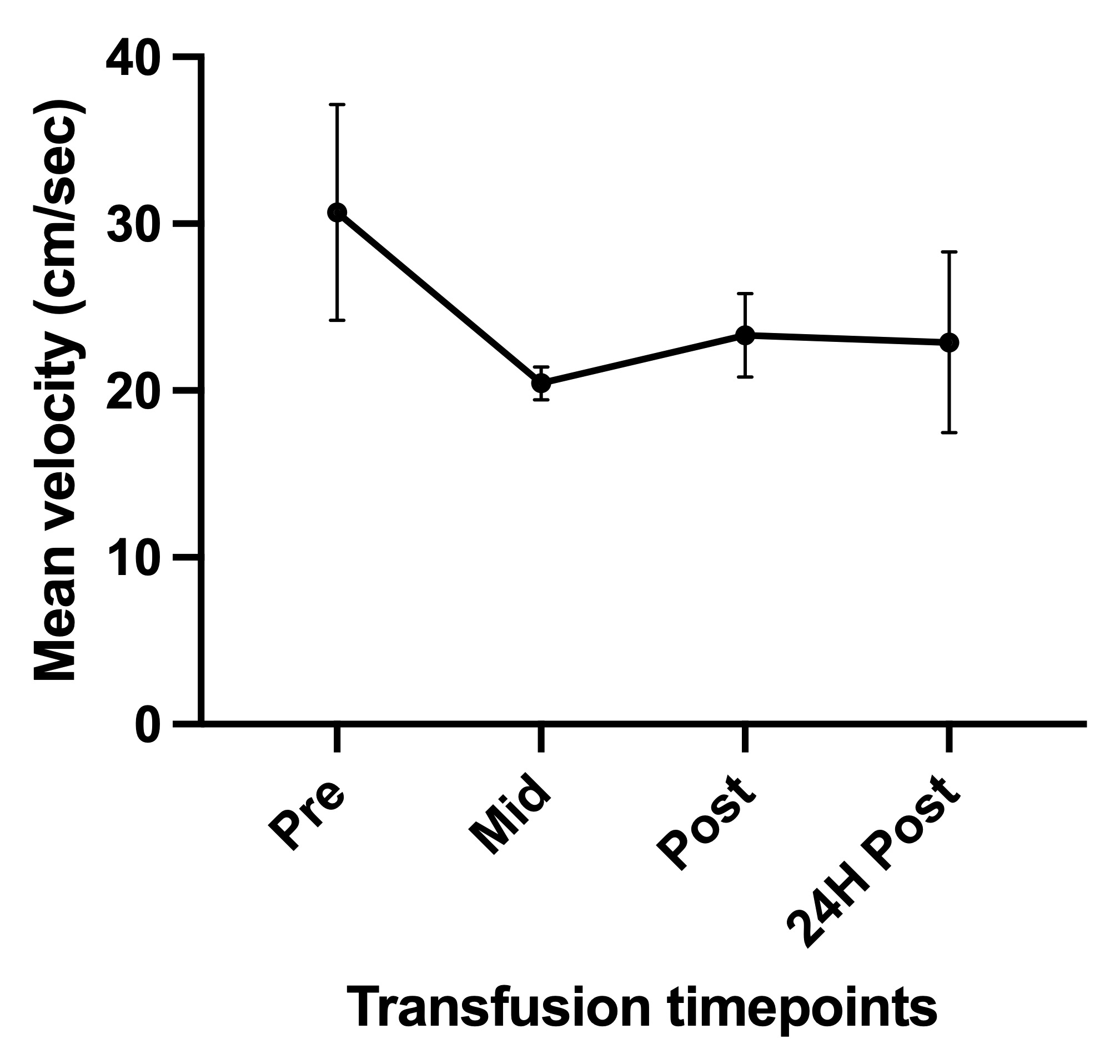
Results: Sixteen infants (BW: 943 ± 283 g, GA: 27.6 ± 1.9 weeks) were enrolled. Thirteen infants were exposed to antenatal betamethasone and ten infants to magnesium prior to delivery, while four had delayed cord clamping for 60 seconds. Mean Apgars at 1 and 5 minutes were 5 ± 2 and 7 ± 2, respectively. Overall, there was a significant increase in MBP, PSV, EDV, and MV (Figure 1A) from DOL 1 to 3 (RM-ANOVA, all p < 0.05) but no significant change in HR. There was no correlation between MBP and CBF measures, but there was a significant negative correlation between hematocrit and MV (polynomial fit, r:-0.512 p: < 0.001), Figure 1B. Four infants received PRBC transfusion. Pre-transfusion CBF was notable for a higher MV (anemic state), followed by a mean decline of 31.1±7.5% mid-transfusion and 21.8±8.2% post-transfusion (RM-ANOVA, p < 0.05) compared to baseline. Twenty-four hours post-transfusion MV was not significantly different from pre-transfusion levels. (Figure 1C). Four infants developed grade II IVH, two of whom received a PRBC transfusion.
Conclusion(s): CBF increased from DOL 1 to DOL 3. Progressively anemic patients demonstrated a pronounced increase in CBF which was followed by a significant decline during the transfusion period. Further studies are needed to determine if the degree of CBF increase in the anemic state is a key contributor to cerebral hemodynamic compromise and subsequent IVH.