Emergency Medicine: All Areas
Emergency Medicine 1
15 - Bacteremia in children diagnosed with pneumonia in emergency departments: A multinational prospective cohort study
Publication Number: 15.11

Mark I. Neuman, MD (he/him/his)
Emergency Medicine
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Globally, blood cultures are commonly obtained in children presenting to emergency departments (ED’s) with community-acquired pneumonia (CAP). The current prevalence and etiology of bacteremia are not well described for this population.
Objective: To assess the prevalence and etiology of bacteremia among children diagnosed with CAP in a global cohort of ED’s.
Design/Methods:
This was a prospective cohort study of children 3 months to < 14 years old with CAP at 69 ED’s in a global consortium, the Pediatric Emergency Research Network. We excluded children with hospitalizations within the previous 7 days, hospital-acquired pneumonias, or chronic complex conditions. Bacteremia was defined by pathogen detection in blood culture. Patient demographics, clinical characteristics, radiographic findings, and laboratory testing results were compared between children with and without bacteremia.
Results:
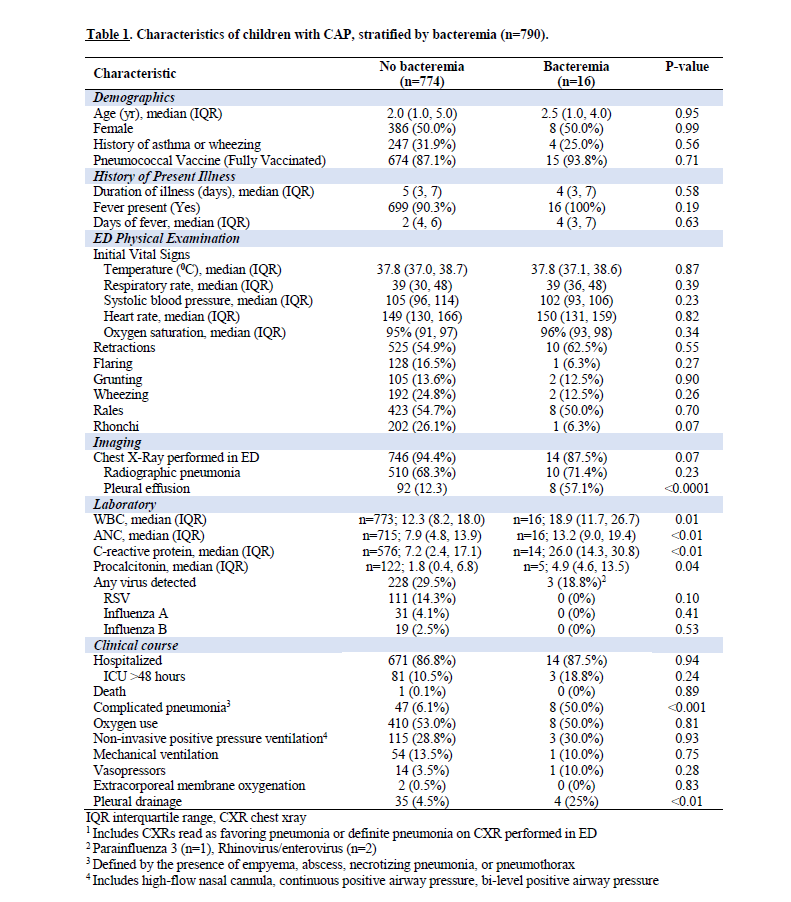
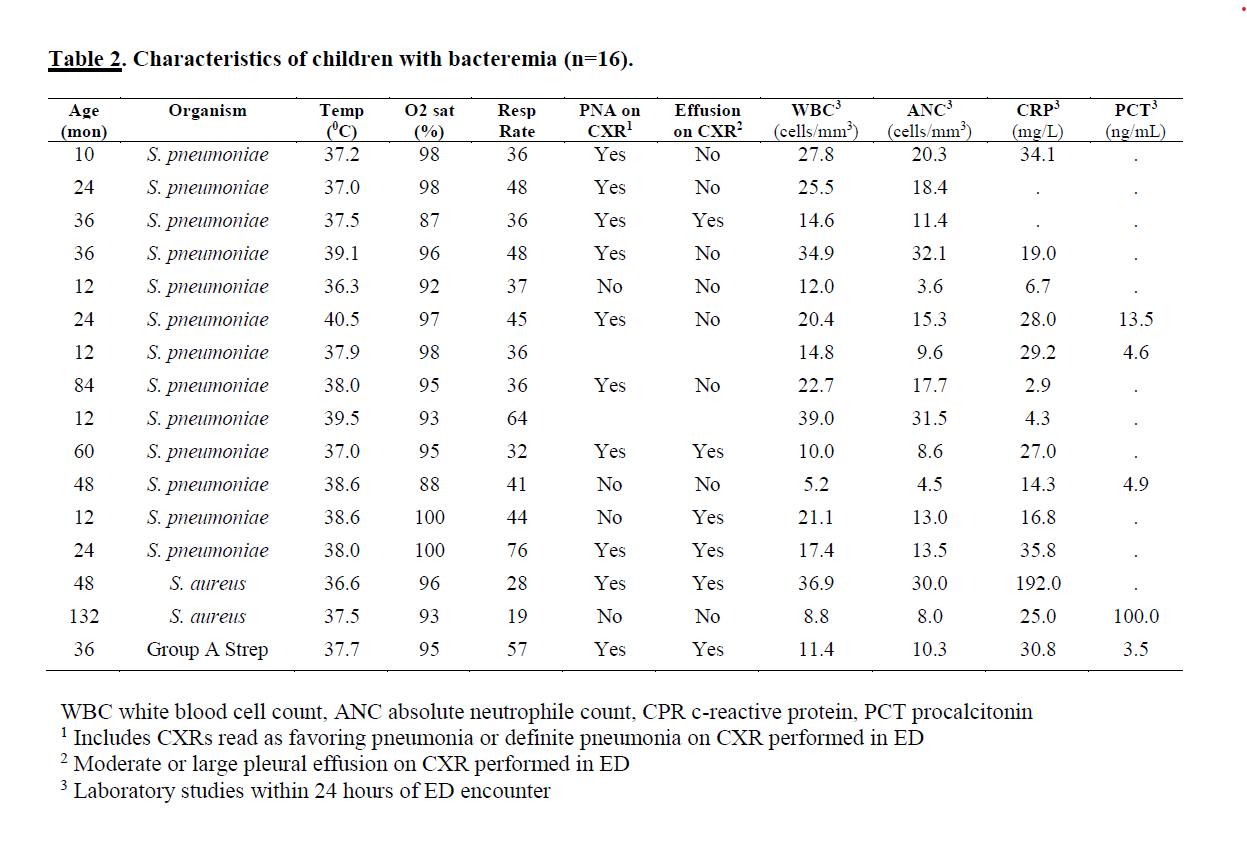
A total of 2,540 children (median age 3.8 years) with CAP were enrolled. Blood cultures were obtained from 790 (31.1%) patients, and 16 (2.0%) demonstrated growth of a pathogen. Streptococcus pneumoniae accounted for 13 (81.3%) cases of bacteremia, Staphylococcus aureus was identified in 2 patients, and Group A streptococcus in 1. Clinical and radiographic findings did not significantly differ between children with and without bacteremia; however, inflammatory markers were significantly higher among children with bacteremia. (Table 1) Eight children with bacteremia had complicated pneumonias, 6 had moderate-to-large pleural effusions, and 4 underwent pleural drainage. (Table 2)
Conclusion(s): Bacteremia is uncommon among children diagnosed with CAP in the ED globally. Although our study demonstrates clinical and radiographic findings are similar between children with and without bacteremia, inflammatory markers are significantly higher among children with bacteremia.